References
1. Briggs A. M., de Carvalho I. A.. 2018;Actions required to implement integrated care for older people in the community using the World Health Organization’s ICOPE approach: A global Delphi consensus study. PLOS ONE 13(10):e0205533.
https://doi.org/10.1371/journal.pone.0205533.
2. Kessler R. C., Davis R. B., Foster D. F., Van Rompay M. I., Walters E. E., Wilkey S. A., Kaptchuk T. J., Eisenberg D. M.. 2001;Long-term trends in the use of complementary and alternative medical therapies in the United States. Annals of Internal Medicine 135(4):262–268.
https://doi.org/10.7326/0003-4819-135-4-200108210-00011.
3. Ayele A. A., Tegegn H. G., Haile K. T., Belachew S. A., Mersha A. G., Erku D. A.. 2017;Complementary and alternative medicine use among elderly patients living with chronic diseases in a teaching hospital in Ethiopia. Complementary Therapies in Medicine 35:115–119.
https://doi.org/10.1016/j.ctim.2017.10.006.
4. Takayama S., Iwasaki K.. 2017;Systematic review of traditional Chinese medicine for geriatrics. Geriatrics & Gerontology International 17(5):679–688.
https://doi.org/10.1111/ggi.12803.
6. Walton M. K., Powers J. H., Hobart J., Patrick D. L., Marquis P., Vamvakas S., Isaac M., Molsen E., Cano S. J., Burke L.. 2015;Clinical Outcome Assessments: Conceptual Foundation–Report of the ISPOR Clinical Outcomes Assessment – Emerging Good Practices for Outcomes Research Task Force DOES THIS HAVE TO BE LABLED AS PART 1. Value in Health : The Journal of the International Society for Pharmacoeconomics and Outcomes Research 18(6):741–752.
https://doi.org/10.1016/j.jval.2015.08.006.
7. Bang G., Kang D., Cho J.. 2022;Current status of routine use of Patient-Reported Outcome in the tertiary hospital clinical setting in Republic of Korea. Korean Journal of Clinical Pharmacy 32(2):74–83.
https://doi.org/10.24304/kjcp.2022.32.2.74.
9. Eton D. T., Bauer B. A., Sood A., Yost K. J., Sloan J. A.. 2011;Patient-Reported Outcomes in Studies of Complementary and Alternative Medicine: Problems, Solutions, and Future Directions. EXPLORE 7(5):314–319.
https://doi.org/10.1016/j.explore.2011.06.002.
10. Barnes P. M., Bloom B., Nahin R. L.. 2008;Complementary and alternative medicine use among adults and children: United States, 2007. National Health Statistics Reports 12:1–23.
12. Paterson C., Baarts C., Launsø L., Verhoef M. J.. 2009;Evaluating complex health interventions: A critical analysis of the “outcomes” concept. BMC Complementary and Alternative Medicine 9:18.
https://doi.org/10.1186/1472-6882-9-18.
15. Hays R. D., Weech-Maldonado R., Teresi J. A., Wallace S. P., Stewart A. L.. 2018;Commentary: Copyright Restrictions versus Open Access to Survey Instruments. Medical Care 56(2):107–110.
https://doi.org/10.1097/MLR.0000000000000857.
16. Ongenae K., Dierckxsens L., Brochez L., van Geel N., Naeyaert J. M.. 2005;Quality of life and stigmatization profile in a cohort of vitiligo patients and effect of the use of camouflage. Dermatology (Basel, Switzerland) 210(4):279–285.
https://doi.org/10.1159/000084751.
18. Anfray C., Arnold B., Martin M., Eremenco S., Patrick D. L., Conway K., Acquadro C., ; ISOQOL Translation and Cultural Special Interest Group (TCA-SIG). 2018;Reflection paper on copyright, patient-reported outcome instruments and their translations. Health and Quality of Life Outcomes 16(1):224.
https://doi.org/10.1186/s12955-018-1050-4.
21. Herdman M., Gudex C., Lloyd A., Janssen M., Kind P., Parkin D., Bonsel G., Badia X.. 2011;Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation 20(10):1727–1736.
https://doi.org/10.1007/s11136-011-9903-x.
22. Nasreddine Z. S., Phillips N. A., Bédirian V., Charbonneau S., Whitehead V., Collin I., Cummings J. L., Chertkow H.. 2005;The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. Journal of the American Geriatrics Society 53(4):695–699.
https://doi.org/10.1111/j.1532-5415.2005.53221.x.
23. McKown S., Acquadro C., Anfray C., Arnold B., Eremenco S., Giroudet C., Martin M., Weiss D.. 2020;Good practices for the translation, cultural adaptation, and linguistic validation of clinician-reported outcome, observer-reported outcome, and performance outcome measures. Journal of Patient-Reported Outcomes 4(1):89.
https://doi.org/10.1186/s41687-020-00248-z.
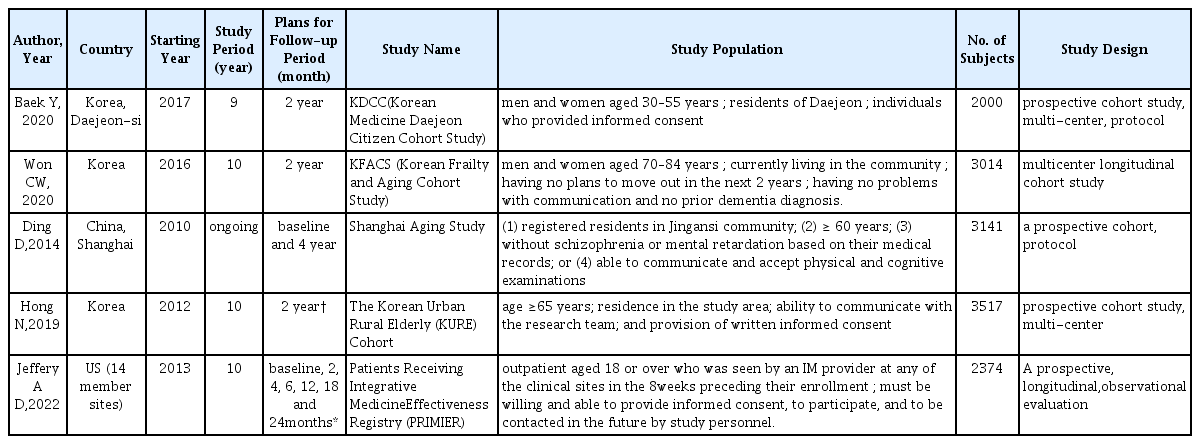
24. Won C. W., Lee S., Kim J., Chon D., Kim S., Kim C.-O., Kim M. K., Cho B., Choi K. M., Roh E., Jang H. C., Son S. J., Lee J.-H., Park Y. S., Lee S.-G., Kim B. J., Kim H. J., Choi J., Ga H., Kim M.. 2020;Korean frailty and aging cohort study (KFACS): Cohort profile. BMJ Open 10(4):e035573.
https://doi.org/10.1136/bmjopen-2019-035573.
25. Ding D., Zhao Q., Guo Q., Meng H., Wang B., Yu P., Luo J., Zhou Y., Yu L., Zheng L., Chu S., Mortimer J. A., Borenstein A. R., Hong Z.. 2014;The Shanghai Aging Study: Study design, baseline characteristics, and prevalence of dementia. Neuroepidemiology 43(2):114–122.
https://doi.org/10.1159/000366163.
26. Hong N., Kim K.-J., Lee S. J., Kim C. O., Kim H. C., Rhee Y., Youm Y., Choi J.-Y., Park H.-Y.. 2019;Cohort profile: Korean Urban Rural Elderly (KURE) study, a prospective cohort on ageing and health in Korea. BMJ Open 9(10):e031018.
https://doi.org/10.1136/bmjopen-2019-031018.
27. Baek Y., Seo B.-N., Jeong K., Yoo H., Lee S.. 2020;Lifestyle, genomic types and non-communicable diseases in Korea: A protocol for the Korean Medicine Daejeon Citizen Cohort study (KDCC). BMJ Open 10(4):e034499.
https://doi.org/10.1136/bmjopen-2019-034499.
28. Dusek J. A., Abrams D. I., Roberts R., Griffin K. H., Trebesch D., Dolor R. J., Wolever R. Q., McKee M. D., Kligler B.. 2016;Patients Receiving Integrative Medicine Effectiveness Registry (PRIMIER) of the BraveNet practice-based research network: Study protocol. BMC Complementary and Alternative Medicine 16:53.
https://doi.org/10.1186/s12906-016-1025-0.
29. Kim S.-H., Jo M.-W., Ahn J., Ock M., Shin S., Park J.. 2014;Assessment of psychometric properties of the Korean SF-12 v2 in the general population. BMC Public Health 14:1086.
https://doi.org/10.1186/1471-2458-14-1086.
30. Yang S.. 1992;Effects of Fluid Intake, Dietary Fiber Supplement and Abdominal Muscle Exercises on Antipsychotic Drug-Induced Constipation in Schizophrenics. Journal of Catholic Medical College 45(4):1501–1514.
32. KEE B. S.. 1996;A Preliminary Study for the Standardization of Geriatric Depression Scale Short Form-Korea Version. J Korean Neuropsychiatr Assoc 35(2):298–306.
34. Won C. W., Yang K. Y., Rho Y. G., Kim S. Y., Lee E. J., Yoon J. L., Cho K. H., Shin H. C., Cho B. R., Oh J. R., Yoon D. K., Lee H. S., Lee Y. S.. 2002;The Development of Korean Activities of Daily Living(K-ADL) and Korean Instrumental Activities of Daily Living(K-IADL) Scale. Journal of the Korean Geriatrics Society 6(2):107–120.
35. Lawton M. P., Brody E. M.. 1969;Assessment of older people: Self-maintaining and instrumental activities of daily living. The Gerontologist 9(3):179–186.
36. Resnick B., Galik E., Dorsey S., Scheve A., Gutkin S.. 2011;Reliability and validity testing of the physical resilience measure. The Gerontologist 51(5):643–652.
https://doi.org/10.1093/geront/gnr016.
37. Park G., Cho B., Kwon I. S., Park B. J., Kim T., Cho K. Y., Park U. J., Kim M. J.. 2016;Reliability and Validity of Korean Version of Falls Efficacy Scale-International (KFES-I). Journal of Korean Academy of Rehabilitation Medicine 34(5):554–559.
38. Yardley L., Beyer N., Hauer K., Kempen G., Piot-Ziegler C., Todd C.. 2005;Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age and Ageing 34(6):614–619.
https://doi.org/10.1093/ageing/afi196.
39. Sohn S. I., Kim D. H., Lee M. Y., Cho Y. W.. 2012;The reliability and validity of the Korean version of the Pittsburgh Sleep Quality Index. Sleep & Breathing = Schlaf & Atmung 16(3):803–812.
https://doi.org/10.1007/s11325-011-0579-9.
40. Buysse D. J., Reynolds C. F., Monk T. H., Berman S. R., Kupfer D. J.. 1989;The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research 28(2):193–213.
https://doi.org/10.1016/0165-1781(89)90047-4.
41. Craig C. L., Marshall A. L., Sjöström M., Bauman A. E., Booth M. L., Ainsworth B. E., Pratt M., Ekelund U., Yngve A., Sallis J. F., Oja P.. 2003;International physical activity questionnaire: 12-country reliability and validity. Medicine and Science in Sports and Exercise 35(8):1381–1395.
https://doi.org/10.1249/01.MSS.0000078924.61453.FB.
42. Oh J. Y., Yang Y. J., Kim B. S., Kang J. H.. 2007;Validity and Reliability of Korean Version of International Physical Activity Questionnaire (IPAQ) Short Form. Journal of the Korean Academy of Family Medicine 28(7):532–541.
43. Rubenstein L. Z., Harker J. O., Salvà A., Guigoz Y., Vellas B.. 2001;Screening for undernutrition in geriatric practice: Developing the short-form mini-nutritional assessment (MNA-SF). The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 56(6):M366–372.
https://doi.org/10.1093/gerona/56.6.m366.
44. Wilson M.-M. G., Thomas D. R., Rubenstein L. Z., Chibnall J. T., Anderson S., Baxi A., Diebold M. R., Morley J. E.. 2005;Appetite assessment: Simple appetite questionnaire predicts weight loss in community-dwelling adults and nursing home residents. The American Journal of Clinical Nutrition 82(5):1074–1081.
https://doi.org/10.1093/ajcn/82.5.1074.
45. Oh S. Y., Koh S.-J., Yeon B. J., Kwon K. A., Jeung H.-C., Lee K. H., Young-Woong W., Lee H. J.. 2019;Validity and Reliability of Korean Version of Simplified Nutritional Appetite Questionnaire in Patients with Advanced Cancer: A Multicenter, Longitudinal Study. Cancer Research and Treatment 51(4):1612–1619.
47. Lim M. K., Kim M. H., Shin Y. J., Yoo W. S., Yang B. M.. n.d;Social Support and Self-rated Health Status in a Low Income Neighborhood of Seoul, Korea. Journal of Preventive Medicine and Public Health 36(1):54–62.
49. Su J. E., Yun Y. G., Ryong Y. H., Kim I. C., Park J.-Y., Jung I.. 2017;Preliminary Study to Develop the Instrument of Korean Medical Pattern Identification and Functional Evaluation for Five Organ. Journal of Physiology & Pathology in Korean Medicine 31(2):126–137.
https://doi.org/10.15188/kjopp.2017.04.31.2.126.
50. Kang B.-K., Jang S., Ko M. M., Jung J.. 2019;A Study on the Development of a Korean Metabolic Syndrome Questionnaire Using Blood Stasis Clinical Data. Evidence-Based Complementary and Alternative Medicine: eCAM 2019;:8761417.
https://doi.org/10.1155/2019/8761417.
51. Cheong M. J., Lee G.-E., Lee Y., Bae K.-H., Kang Y., Kim J.-H., Lyu Y.-S., Kang H. W.. 2019;Validation of the Core Seven-Emotions Inventory—Short form. Integrative Medicine Research 8(2):116–119.
https://doi.org/10.1016/j.imr.2019.04.003.
52. Lee J.-Y., Dong Woo Lee null, Cho S.-J., Na D. L., Hong Jin Jeon null, Kim S.-K., You Ra Lee null, Youn J.-H., Kwon M., Lee J.-H., Maeng Je Cho null. 2008;Brief screening for mild cognitive impairment in elderly outpatient clinic: Validation of the Korean version of the Montreal Cognitive Assessment. Journal of Geriatric Psychiatry and Neurology 21(2):104–110.
https://doi.org/10.1177/0891988708316855.
55. Guralnik J. M., Simonsick E. M., Ferrucci L., Glynn R. J., Berkman L. F., Blazer D. G., Scherr P. A., Wallace R. B.. 1994;A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. Journal of Gerontology 49(2):M85–94.
https://doi.org/10.1093/geronj/49.2.m85.
56. McGill S. M., Childs A., Liebenson C.. 1999;Endurance times for low back stabilization exercises: Clinical targets for testing and training from a normal database. Archives of Physical Medicine and Rehabilitation 80(8):941–944.
https://doi.org/10.1016/s0003-9993(99)90087-4.
58. Demers L., Ska B., Desrosiers J., Alix C., Wolfson C.. 2004;Development of a conceptual framework for the assessment of geriatric rehabilitation outcomes. Archives of Gerontology and Geriatrics 38(3):221–237.
https://doi.org/10.1016/j.archger.2003.10.003.
59. Prorok J. C., Williamson P. R., Shea B., Rolfson D., Mañas L. R., Cesari M., Kim P., Muscedere J.. 2022;An international Delphi consensus process to determine a common data element and core outcome set for frailty: FOCUS (The Frailty Outcomes Consensus Project). BMC Geriatrics 22(1):284.
https://doi.org/10.1186/s12877-022-02993-w.
60. U.S. Department of Health and Human Services FDA Center for Drug Evaluation and Research, U.S. Department of Health and Human Services FDA Center for Biologics Evaluation and Research, & U.S. Department of Health and Human Services FDA Center for Devices and Radiological Health. 2006;Guidance for industry: Patient-reported outcome measures: use in medical product development to support labeling claims: draft guidance. Health and Quality of Life Outcomes 4(1):79.
https://doi.org/10.1186/1477-7525-4-79.
61. Al Sayah F., Jin X., Johnson J. A.. 2021;Selection of patient-reported outcome measures (PROMs) for use in health systems. Journal of Patient-Reported Outcomes 5(Suppl 2):99.
https://doi.org/10.1186/s41687-021-00374-2.
62. Revicki D. A., Schwartz C. E.. 2009;Intellectual property rights and good research practice. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation 18(10):1279–1280.
https://doi.org/10.1007/s11136-009-9551-6.
64. Williamson P. R., Altman D. G., Blazeby J. M., Clarke M., Devane D., Gargon E., Tugwell P.. 2012;Developing core outcome sets for clinical trials: Issues to consider. Trials 13(1):132.
https://doi.org/10.1186/1745-6215-13-132.
66. Williamson P. R., Altman D. G., Blazeby J. M., Clarke M., Devane D., Gargon E., Tugwell P.. 2012;Developing core outcome sets for clinical trials: Issues to consider. Trials 13:132.
https://doi.org/10.1186/1745-6215-13-132.