Availability of Diagnosis of Yin-deficiency in Elderly People with Xerostomia and Factors Influencing Subjective Oral Dryness: A Prospective Cross-sectional Study
Article information
Abstract
Objectives:
The aims of this study were to investigate the availability of diagnosis of Yin-deficiency in the elderly with xerostomia and factors influencing subjective oral dryness.
Methods:
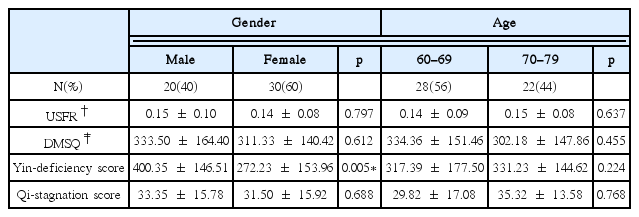
We surveyed 50 patients recruited by the clinical trial, ‘Efficacy of Yukmijihwang-tang on Xerostomia in the Elderly: A Randomized, Double-blind, Placebo-controlled, Two-center Trial’. The subjects were assessed on their subjective oral dryness using the Dry Mouth Symptom Questionnaire (DMSQ). Their salivary functions were measured by Unstimulated Salivary Flow Rate (USFR) measurements. In addition, the subjects were evaluated on their Qi-stagnation and Yin-deficiency conditions using the Qi-stagnation questionnaire and Yin-deficiency questionnaire.
Results:
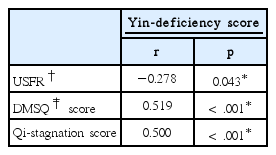
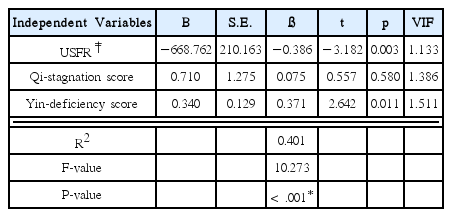
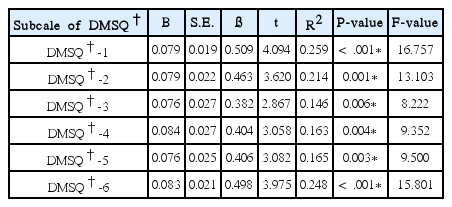
There were statistically significant correlations between three variables (USFR, DMSQ score and Qi-stagnation score) and Yin-deficiency score. In the multiple regression analysis, the regression model was statistically significant (F = 10.273, p < .001). The factor most strongly influencing the subjective oral dryness was USFR (ß = −0.386). Yin-deficiency had the next strongest impact on the subjective oral dryness (ß = 0.371). Qi-stagnation affected the subjective oral dryness weakly (ß = 0.075). In the simple regression analysis, Yin-deficiency had a statistically significant effect on each of six subscales of DMSQ (p < .01). Among the six subscales, DMSQ-1 (‘Oral dryness at night or on awakening’) was the most strongly influenced by Yin-deficiency.
Conclusions:
The results of this study show that the diagnosis of Yin-deficiency in the elderly with xerostomia was available and Yin-deficiency was an important factor influencing the subjective oral dryness. Therefore, the consideration of Yin-deficiency is significant for diagnosis and treatment in the elderly with xerostomia.