References
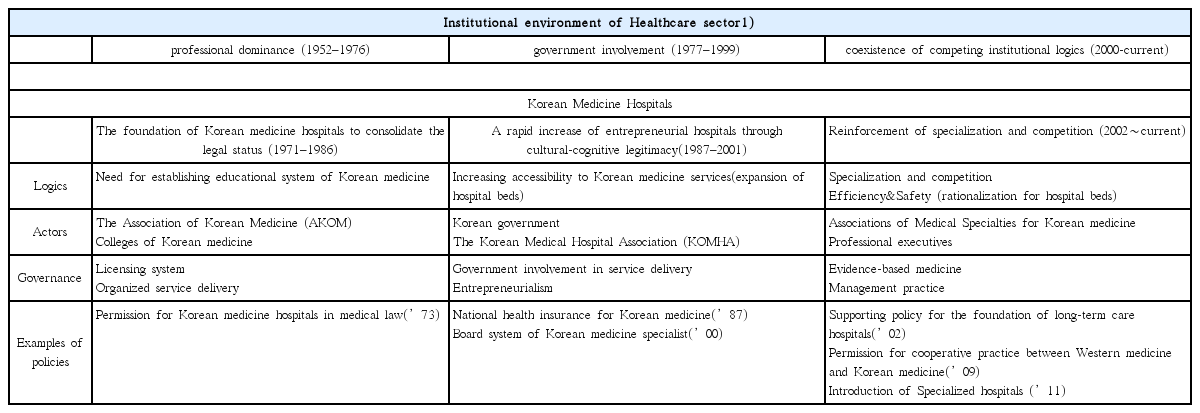
1. Kim SJ, kwon SM, You MS. An Institutional and Ecologial Analysis of the Healthcare Environment in Korea: Focus on Institutional Logics, Actors, and Governance structures. Korean Journal of Health Policy & Adminiatration 2011;21(3):457–92.
2. DiMaggio PJ, Powell WW. The Iron Cage Revisited: Institutional Isomorphism and Collective Rationality in Organizational Fields. American Sociological Review 1983;48(2):147–60.
3. Hannan MT, Freeman J. POPULATION ECOLOGY OF ORGANIZATIONS. American Journal of Sociology 1977;82(5):929–64.
4. D’Aunno T, Sutton RI, Price RH. Isomorphism and external support in conflicting institutional environments: A study of drug abuse treatment units. Academy of Management Journal 1991;34(3):636–61.
5. Scott WR. Organizations : rational, natural, and open systems 5th edth ed. New Jersey: Prentice Hall; 2003. p. 1–430.
6. Scott WR. The Adolescence of Institutional Theory. Administrative Science Quarterly 1987;32(4):493–511.
7. Cho BH. The Sociology of diseases and medicine Seoul: Jipmoondang; 2006. p. 1–639.
8. Scott WR. Institutional change and healthcare organizations : from professional dominance to managed care Chicago: University of Chicago Press; 2000. p. 1–427.
9. Lee HJ, Sung HJ, Cho BH. An analysis of the status Change of Korean Oriental Medicine. Journal of Korea Institute of Oriental Medicine 1999;5(1):133–9.
10. Yi GM. A Study on the General Public Understanding and Utilization of Korean Traditional Medicine in Colonial Period. Korean J Med Hist 2006;15(2):227–36.
11. Shin DW. Traditional Medicine under Japanese Rule after 1930s. J Kor Med History 2003;12(2):110–28.
12. Korean Oriental Medical Association. The 40-Year History of the Korean Oriental Medical Association 1989.
13. Jung WY. The 100 years’ history of Korean medicine. J Kor Med History 1999;8(2):169–86.
14. Korean Institute of Oriental Medicine. The Reestablishment of the history of Korean Medicine Seoul: Korean Institute of Oriental Medicine; 1995.
15. Association of Korean Medicine. 1898–2011 The history of Korean medicine association 2012.
16. committee Hc. the 30 years’ history of Kyunghee hopsipital. 2012.
17. Yoon JS. A Study on the Management Strategies of the Small Oriental Medical Hospitals [dissertation] Seoul: Kyung Hee University; 2000.
18. Cho BH. The State Control of Medicine and Medical Profession. Journal of Korean Sociological Association 1990;24(1):1131–53.
19. Reston J. Now, About My Operation in Peking. New York Times 1971;Jul. 26.
20. You WG. A Study on Utilization Pattern and Determinants of Oriental Medical Services, in Health policy & administration Seoul National University; 2002.
21. Lee HJ. Comparative Study of the National Policies for Korean Oriental Medicine and Traditional Chinese Medicine. Korean J. Oriental Physiology & Pathology 2008;22(5):1132–9.
22. Department of Health and Welfare. Korea Health Industry Development Institution, Health Technology Research Planning Evaluation Board, 2002 giude of Korean medicine Remedies Research & Development ed. Department of Health and Welfare. 2002.
23. Department of Health and Welfare. The Introduction of traditional medicine policy, Department of Health and Welfare, Editor. 1999.
24. Kang BJ, Chae BJ, Kwon DH, Kim PT, Kim JS. Survey on the Understanding of Modern vs. Oriental Medicine in Korea. J Korean Society of Biological Therapies in Psychiatry 1999;5(2):158–66.
25. Nam JJ, Choi JS, Kim JH, Moon SS. National Health and Nutrition Examination Survey In-depth and Related analysis. Department of Health and Welfare, Korea Institute for Health and Social Affairs 2000;:1–399.
26. Kwon SS, Oh CD, Yang SY, Lee HH, Kang HC, Jung ES. Basic Survey on the Patients’ cognition and satisfaction with Western and Oriental Medicine. The Journal of the Korean Academy of Family Medicine 1992;13(11):891–900.
27. Nah YS. Study on the attributes of Patients admitted to western and oriental medical hospitals of Kyung-Hee university medical center [dissertation] Seoul: Kyung Hee University; 1990.
28. Go SK, Jeun HN, Park DJ, Min JH, Kim JH. New role of oriental hospital in the aging society, Health Insurance Review and Assessment Service 2005.
29. Do YK. analysis of hospital bed policies in Korea : Focused on the comparison between U.S., Japan, and Korea, in Graduate School of Public Health, Seoul Nationtl University. 2003.
30. Korea Institute of Oriental Medicine. Comparative Research on Traditional medicine Policy in Korea and Asian 3 Countries, Korea Institute of Oriental Medicine. 1997.
31. Lee JY, Park EK, Yoon JY, Song SH. Report on the Operating Status of Long-tern Care Hospitals, Department of Health and Welfare, Health Insurance Review and Assessment 2007;
32. Chung KH, Cho BS. A study on the field survey of domestic long-term hospitals facilities. JOURNAL OF THE ARCHITECTURAL INSTITUTE OF KOREA Planning &Design 2003;19(9):3–11.
33. Kim DY. Establishment of policy for Korean medicine in long-term care. Akomnews 2007;Nov. 19.
34. Han DW, Lim BM. The Role of Public Health in Korean Medicine for Aging Society, Department of Health and Welfare 2005;