References
1. Francisco GE, McGuire JR. Poststroke spasticity management. Stroke; a journal of cerebral circulation 2012;43(11):3132–6.
2. Kim YH, Han TR, Jung HY, Chun MH, Lee JM, Kim DY, et al. Clinical Practice Guideline for Stroke Rehabilitation in Korea. Brain & Neuro Rehabilitation 2009;2(1):1–38.
3. VA/DOD Clinical practice guideline for the management of stroke rehabilitation. Journal of rehabilitation research and development 2010;47(9):1–43.
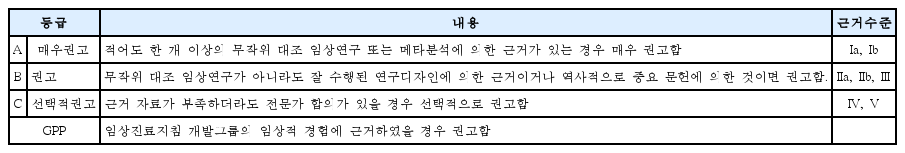
4. Lee MS. Recommendations for Development of Clinical Practice Guideline in Korean Medicine (PRIDE-CPG-KM). Korea Institute of Oriental Medicine 2013;
5. Park SW, Yi SH, Lee JA, Hwang PW, Yoo HC, Kang KS. Acupuncture for the treatment of spasticity after stroke: a meta-analysis of randomized controlled trials. J Altern Complement Med 2014;20(9):672–82.
6. Moon SK, Whang YK, Park SU, Ko CN, Kim YS, Bae HS, et al. Antispastic effect of electroacupuncture and moxibustion in stroke patients. The American journal of Chinese medicine 2003;31(3):467–74.
7. Lee SW, Yun JM, Son JW, Kang BG, Park SM, Yun HJ, et al. The Effect of Electroacupuncture on Upper-Extremity Spasticity of Stroke Patients. Journal of Korean oriental internal medicine 2007;28(3):492.
8. Gong WJ, Zhang T, Cui LH. Effects of Electroacupuncture at Zusanli (ST36) on Lower Limbs Motor Function in Patients with Stroke during Spasm Period:A Clinical Research. Chinese Journal of Rehabilitation Theory and Practice 2008;14(11):1057–8.
9. Li L, Yang WX, Hu FJ. Clinical Effect of Electric Acupuncture and Baclofen on Recovery of Spasticity. Chinese Journal of Rehabilitation 2007;22(5):319–20.
10. Zong T. Influence of Du Acupoint Electrical Stimulation on Limb Spasticity after Cerebral Infarction and Motor Function. Liaoning Journal of Traditional Chinese Medicine 2012;39(7):1391–3.
11. Park DS, Choi DY, Lee JD, Kim YS, Nam SS, Lee SH, et al. The Acupuncture and Moxibustion Medicine. Jipmoondang 2012;601
12. Fink M, Rollnik JD, Bijak M, Borstadt C, Dauper J, Guergueltcheva V, et al. Needle acupuncture in chronic poststroke leg spasticity. Archives of physical medicine and rehabilitation 2004;85(4):667–72.
13. Dong XL, Feng XM, Zhu H. Evaluation of the effects of acupuncture for the treatment of hemipleyis in patients with stroke by Fugl-Meyer. Chinese Journal of Clinical Rehabilitation 2003;7(19):2711–2.
14. Zhang ZM, L FC, Pi ZK, Fan XY, Chen HQ, Zhang J. Observation on clinical therapeutic effect of acupuncture on upper limb spasticity in the patient of poststroke. Chinese Acupuncture & Moxibustion 2008;28(4):257–60.
15. Wu HM, Tang JL, Lin XP, Lau JTF, Leung PC, Woo J, et al. Acupuncture for stroke rehabilitation. Cochrane Database of Systematic Reviews 2006;(3):CD004131.
16. Zhao JG, Cao CH, Liu CZ, Han BJ, Zhang J, Li ZG, et al. Effect of acupuncture treatment on spastic states of stroke patients. Journal of the neurological sciences 2009;276(1–2):143–7.
17. Ernst E, White AR. Prospective studies of the safety of acupuncture: a systematic review. The American journal of medicine 2001;110(6):481–5.
18. Kim SY, Ji SM, Lee SJ, Lee YJ, Park JE, Nam MH, et al. Guidance for development of clinical practice guidelines. National Evidence-based Healthcare Collaborating Agency 2011;:20–77.
19. Yoon BW, Hong KS, Kwon SU, Lee SH, Ko SB, Choi HY. Clinical Practice Guidelines for Stroke. Clinical Research Center for Stroke 2013;
20. Rah UW, Kim YH, Ohn SH, Chun MH, Kim MW, Yoo WK, et al. Clinical Practice Guideline for Stroke Rehabilitation in Korea 2012. Brain & Neuro Rehabilitation 2014;7(1(suupl.1)):S1–S75.