Analysis of Herbal-drug-associated Adverse Drug Reactions Using Data from Spontaneous Reporting System in Electronic Medical Records
Article information
Abstract
Objectives:
The purpose of this study was to understand the status of reporting and characteristics of adverse drug reactions (ADRs) induced by herbal drugs and to make a suggestion for the domestic pharmacovigilance system on herbal medicine.
Methods:
We carried out a hospital-based observational study at Dongguk University Ilsan Oriental Hospital from April 2012 to December 2014. We reviewed all the herbal-drug-associated ADRs reports registered to the spontaneous ADR reporting system in electronic medical records of the hospital in the period.
Results:
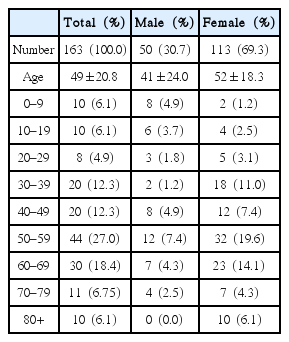
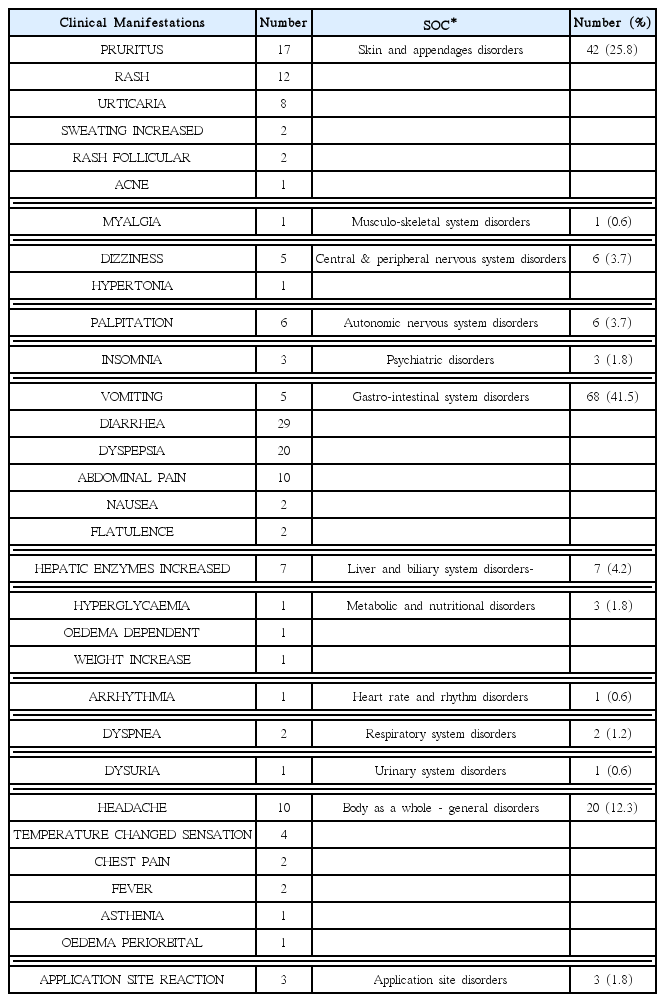
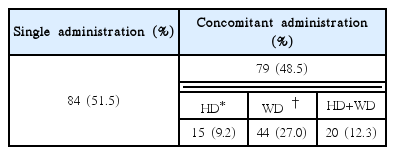
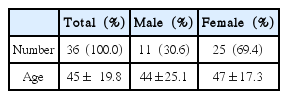
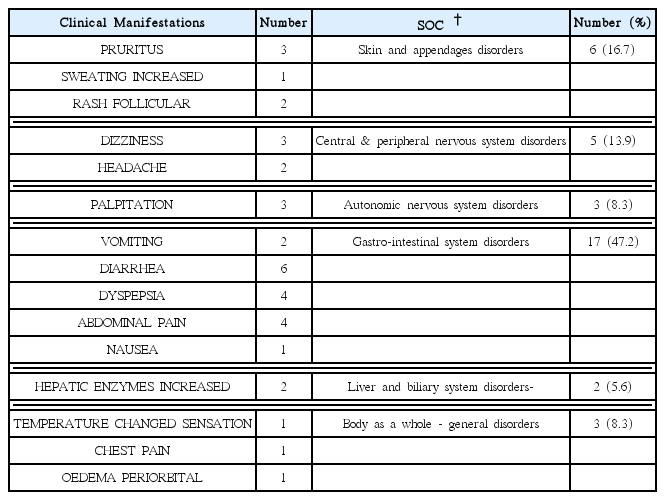
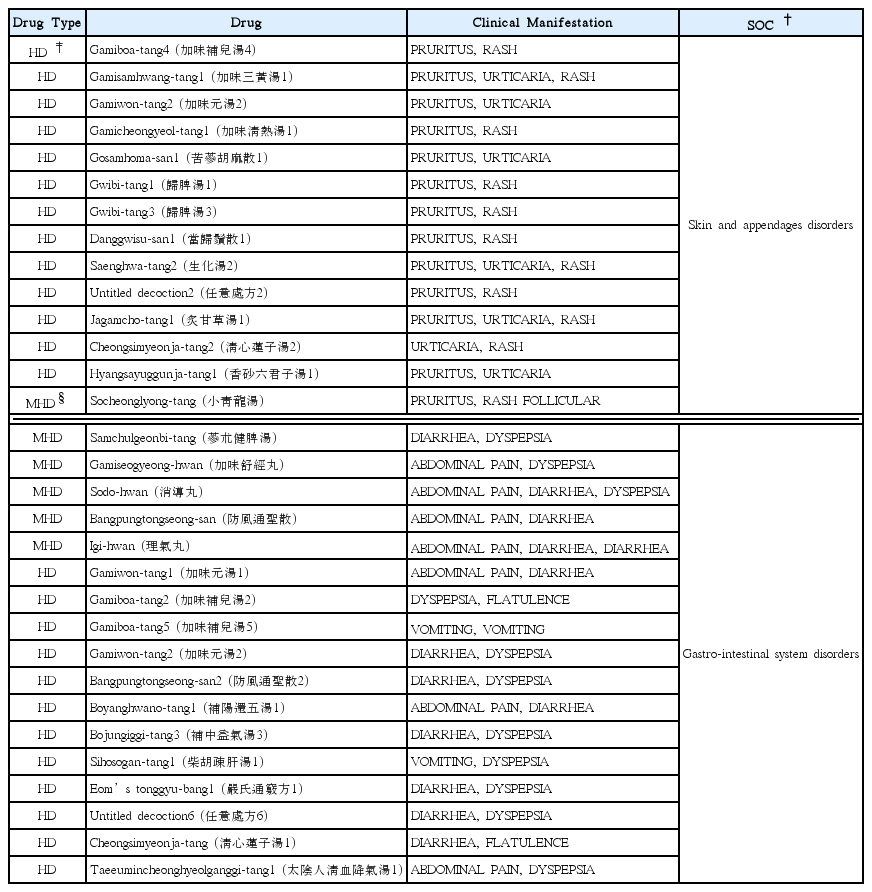
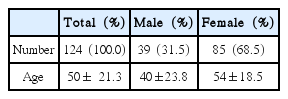
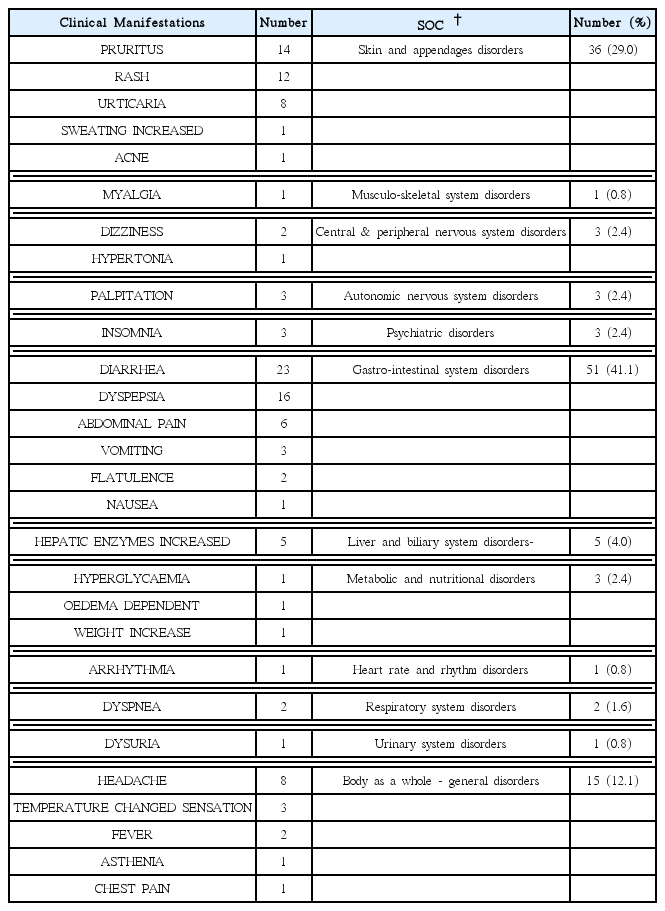
We found out 101 reports including 163 herbal-drug-associated ADRs from 97 patients. Females (69.3%) outnumbered males and the most frequent age group was the 50s (44, 27.0%). No serious adverse event was observed. The most commonly reported ADR was gastro-intestinal system disorders (68, 41.5%) followed by skin-related disorders (42, 25.8%). Diarrhea (29, 17.8%) was the most frequently referred clinical manifestation. Most ADRs were induced by internal medicines (160, 98.2%) including manufactured (36, 22.1%) and self-prepared decoction (160, 76.1%). The pairs of Igi-hwan-diarrhea, gamiboa-tang-vomiting, and Magnoliae Flos-gastro-intestinal-system-related ADRs were observed twice each and the others appeared only once.
Conclusions:
We propose Korean government to take an initiative in national pharmacovigilance system for herbal medicine. To perform the surveillance on herbal drugs, the Association of Korean Medicine (AKOM) should set up a nationwide network by designating centers connecting the Korean medical hospitals, local Korean medicine clinics, and the public health centers. The government and AKOM should also educate and encourage them to understand the pharmacovigilance system and report the ADRs actively.
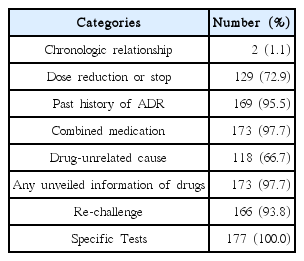
Number of the Cases with No Available Information to Score Each Category of Korean Algorithm for ADR Causality Assessment version 2.0.