A case report of generalized morphea treated with herbal medication and moxibustion
Article information
Abstract
A 56-year-old Korean female patient developed generalized morphea over three months. We focused on imbalance of the neuroendocrine-immune axis, mainly using Jiawei-Renshengyangrong-tang and Jiawei-Siqi-tang. Moxibustion on LU9 was conducted for skin symptoms. The patient’s modified localized scleroderma skin severity index score decreased from 22 to 6 over 22 weeks of treatment and to 4 during a 3-month follow-up. Her verbal rating scale score for general symptoms decreased from 17 to 1 during the 22-week treatment.
Introduction
Generalized morphea is one of five subtypes of localized scleroderma (LS)1), which is a rare disease with an incidence rate of 0.4 to 2.7 per 100,000 people2). Generalized morphea is characterized by morphea exceeding 3 cm in diameter and more than 4 lesions when it involves more than 2 anatomical regions3). Furthermore, it may be accompanied by general symptoms, such as muscle pain, insomnia, heartburn, and fatigue4).
Ultraviolet A1 (UVA) phototherapy is the most commonly recommended treatment1); however, side effects, such as thermal skin burns, itching, and headaches, have been reported, and this treatment has been shown to be unable to relieve general symptoms5). Thus, morphea of large size and morphea involving multiple anatomical regions present greater difficulty for UVA treatment.
In contrast, several studies have demonstrated that alternative therapies might palliate various symptoms induced by the sclerosis6) 7). However, these studies lacked verified outcome measures and definitive diagnoses of the LS subtypes, and they did not aim to clarify the distinctive role of alternative medicine. Although the mechanism of generalized morphea remains unclear, autoimmune mechanisms are strongly believed to be involved. Here, we report the use of moxibustion and Korean herbal medication to modulate the immune system (IS) to improve active generalized morphea.
Case
In Oct 2012, a 56-year-old Korean female patient diagnosed with LS presented to the internal medicine department of a Korean university hospital. She had experienced expanding scleroderma over the course of three months and had previously presented to two other university hospitals, on 10 and 19 Oct 2012, where she was diagnosed with LS based on her symptoms, laboratory tests and a skin biopsy.
The laboratory data collected on 10 Oct revealed positivity for anti-nuclear antibody (ANA), anti-Smith antibody (Ab), and Ro-52, and the results from 19 Oct revealed an ANA titer <1:40, Scl-70 Ab <7.0 U/mL and rheumatoid factor (RF) <10.6 IU/mL. Additionally, a back skin biopsy showed epidermal atrophy with diffuse sclerosis throughout the entire dermis, consistent with scleroderma.
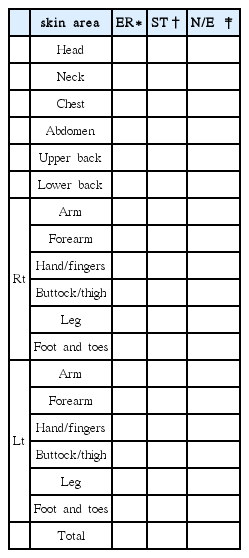
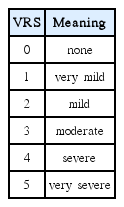
On 31 Oct, the patient’s modified LS skin severity index (mLoSSI)8) score was 22 (Figure 1), and her overall verbal rating scale (VRS) score, which assesses itching, pain, hot flashes, heart burn, fatigue and myalgias, was 17 (Figure 2).
The patient complained of skin pigmentation, itching, a prickly feeling of the skin, and general symptoms, including fatigue, hot flashes, muscle pain and heartburn. The evaluation revealed no evidence of Raynaud’s phenomenon or extended invasion.
mLoSSI scores of the UVA application and non-application sites.
a: UVA application site. b: non-UVA application site. LH: Last HCQ. LU: Last UVA. LM: Last moxibustion
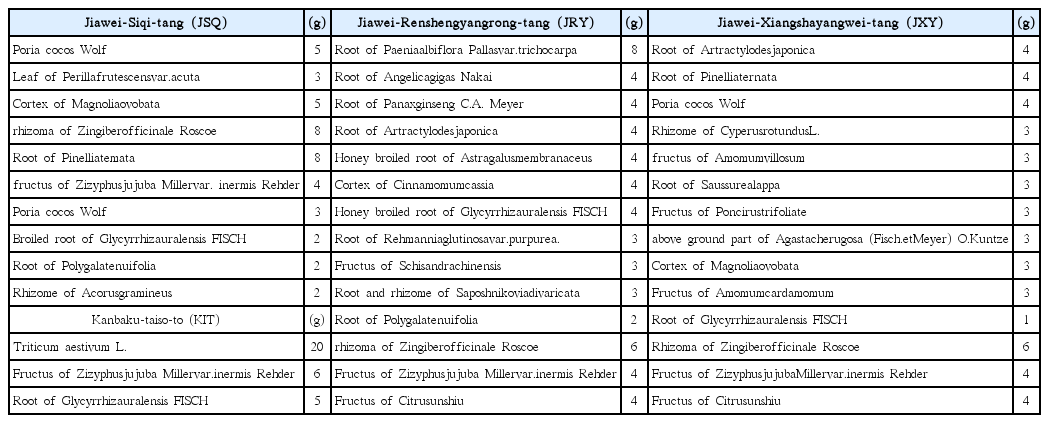
She was considered to have generalized morphea in the active phase, as well as blood deficiency and Qi stagnation based on traditional Korean medicine (TKM), which includes immune disorders. Therefore, we administered moxibustion treatment on LU9 from 29 Oct and Jiawei-Siqi-tang (JSQ: Pusan national Korean medicine hospital (PNUKH), Yangsan, South Korea) qd and Jiawei-Renshengyangrong-tang (JRY: PNUKH, Yangsan, South Korea) bid for 50 days starting from 1 Nov. The patient was also separately and simultaneously administered 100 mg hydroxychloroquine (HCQ) sulfate once daily and UVA phototherapy at 165 J/cm2 at another hospital. Her mLoSSI score decreased from 22 on 31 Oct to 20 on 14 Nov and to 19 on 19 Nov. Additionally, her total VRS score for six subjective symptoms gradually decreased from 17 on 31 Oct to 4 on 30 Nov. Meanwhile, HCQ administration was stopped on 8 Dec both because the patient rejected it and because the treatment aim was unclear. The mLoSSI score of the UVA application site showed no change until 30 Nov, whereas the non-application site score decreased by 3 points. Moreover, the application site had the adverse appearance of a thermal burn, and consequently, the UVA treatment was stopped on 13 Dec 2012 following a total of 31 doses since 17 Oct. Because the patient did not sense any heat and because no skin lesions developed in the early treatment stage, we gradually increased the number of moxibustion treatment layers to seven. She eventually reported a heat sensation and itching at the moxibustion site for the first time on 24 Dec. Thus, we decreased the moxibustion to five layers per visit, and a second-degree burn was observed on 2 Jan after 25 total moxibustion sessions. Thus, the moxibustion treatment was stopped, as was JRY. Jiawei-Xiangshayangwei-tang (JXY: PNUKH, Yangsan, South Korea) bid and JSQ qd were administered for 10 days beginning on 9 Jan because the patient had complained of dyspepsia and chest discomfort, while the subjective skin symptoms and fatigue were diminished. On 31 Jan, her VRS score was reduced to 2, and her mLoSSI score decreased to 4. Kanbaku-taiso-to (KTT; Tsumura & Co., Tokyo, Japan) qd was administered with JSQ bid to address chest discomfort for 15 days, starting from 31 Jan. JSQ and JXY were prescribed again for 15 days starting from 6 Mar. Then, with resolution of the patient’s chest discomfort, all treatments were concluded on 20 Mar, when she exhibited a VRS score of 0 and an mLoSSI score of 6. The follow-up scores were a VRS score of 0 and an mLoSSI score of 4, as recorded on 19 June.
The changes in the mLoSSI score are shown in Figure 1; the changes in the VRS score are shown in Figure 2; and clinical images of the patient’s left thigh, her back, both of her forearms and her anterior chest are shown in Figures 3–6, respectively.
Change in left thigh pigmentation.
a: Pigmentation of the left thigh was relatively dark and obvious on 31 Oct 2012 (a). The color gradually faded over time: 14 Nov 2012 (b), 30 Nov 2012 (c), 31 Jan 2013 (d) and 19 June 2013 (e).
Multiple oval pigmentations on the upper and lower back.
Multiple brown oval pigmentations were observed on the back on 31 Oct 2012 (a) that continuously faded and decreased over time: 14 Nov 2012 (b), 30 Nov 2012 (c), 31 Jan 2013 (d) and 19 June 2013 (e).
Cornification and glossy epidermal changes and pigmentation on both forearms.
Cornification and pigmentations were observed on the dorsal surface of both forearms on 31 Oct 2012 (a) but decreased over time: 14 Nov 2012 (b), 30 Nov 2012 (c), 31 Jan 2013 (d) and 19 June 2013 (e).
Consideration
This is a report of a case of active generalized morphea that occurred as a result of vacuity of both Qi and blood induced by Qi stagnation. This pathology explains autoimmune disease induced by psychological stress.
Previous studies demonstrated that complementary and alternative (CAM) therapies promoted mental and physical health in systemic sclerosis patients9). However, the effects of these therapies on active-phase generalized morphea with both systemic and skin symptoms have not been reported. Moreover, information on the diagnostic details and treatment of this entity using TKM is lacking.
The patient described here had morphea exceeding 3cm in diameter and more than 4 lesions involving 6 anatomical legions, thus we diagnosed her with generalized scleroderma. Furthermore, we could estimate it active phase, because the morphea was developed in last 3 months.
The mLoSSI is a morphea-specific assessment system certified by the Localized Scleroderma Clinical and Ultrasound Study Group (LOCUS). The grading method for the seriousness of localized scleroderma evaluates erythema, skin thickness, and new lesions or lesion extensions on 18 anatomical parts within the last month. The period is limited to 1 month to prevent any errors from occurring8).
She showed rapid improvement for approximately 3 months from 31 Oct to 31 Jan, during which time her mLoSSI score decreased by 13 points, even though the patient was experiencing the active disease phase. The therapeutic effects and mechanisms of her TKM treatments warrant discussion because although UVA treatment was partially combined with TKM treatments, a 0-point reduction occurred at the UVA application site, whereas the score for the non-application site decreased by 3 points during the UVA treatment period.
The patient particularly complained of psychological stress, which may be interpreted as Qi stagnation, and this condition finally developed into dual vacuity of Qi and blood, as indicated by scleroderma. In fact, 80% of patients with autoimmune disease may experience abnormal psychological stress10), and abnormal childhood experiences causing mental trauma may increase autoimmune disease risk and the risk of autoimmune disease-related hospitalization, which is 70% higher for Th1 responses, 80% higher for Th2 responses and 100% higher in rheumatic disease11). Moreover, one study revealed that mental stress activates one of the initial phases of immune-mediated inflammation12).
The patient described here was treated based on this interpretation of the pathology. An analysis using both physiological terms and TKM terms regarding the patient’s pathological state is shown in Figure 7. The first treatment goal was to manage her chronic psychological stress and improve the dual vacuity of Qi and blood induced by this mental stress; JSQ was administered for this purpose. With the use of JSQ to treat Qi stagnation13) have been reported, and these effects are considered to be related to JSY’s serotonin-modifying actions under stress conditions14). In addition, JRY was administered for fatigue and immune imbalance. Notably, the patient responded with improvement in both her fatigue and the dual vacuity of Qi and blood following JRY treatment, which regulates immune function in the presence of this syndrome15). The time during which the use of those two medications was combined was the most active treatment period, as rapid improvement was observed during this time.
Subsequently, even the patient’s severe fatigue and dual vacuity of Qi and blood were improved. However, because functional disorders from accumulated stress persisted, JXY and KTT were administered. A previous study showed JXY to be effective for chest discomfort due to mental stress and especially Qi stagnation16). KTT is effective for improving mental stress induced diseases17).
These herbal medications were employed to treat the causal factors of the patient’s autoimmune disease, but treatment for her skin symptoms was still needed. Various TKM treatment methods have been established for each of the various types and causes of dermatological diseases. In this case, we focused on the “lung governing the skin and hair” theory because the skin’s immune function should be strongly considered in morphea autoimmune disease. “Lung governing the skin and hair” is a traditional TKM principle that signifies the lung as the root of Qi, which is abundant in the skin and hair. From a physiological point of view, this theory may support the lung’s role in protecting and defending the surface of the skin18). Moreover, moxibustion therapy was selected because moxibustion is known to be superior for lung strengthening through the promotion of organ function and blood and Qi circulation19).
This case showed an intriguing increase in heat sensitivity as the treatment progressed, similar to what is observed in scarring moxibustion, which is a traditional moxibustion treatment method. The relationship between body temperature and systemic disease has consistently received substantial amounts of attention20), and thus, the diagnostic and therapeutic meaning of heat sensitivity warrant investigation.
This case report has some limitation. this report presents only one case and does not contain the lab test result after the treatment. Therefore the effectiveness, safety and mechanisms of each treatment element should be verified by basic research and clinical studies.
Summary
This case report demonstrates improvement in the active LS, which is a subtype of generalized morphea, by TKM treatment based on TKM-based pathology and diagnosis. The result of this study implies that mental stress should be considered when treat autoimmune disease, and that TKM-treatment could be a complementary or alternative treatment for autoimmune disease as TKM theory about autoimmune disease includes similar principle with the neuroendocrine-immune axis.
Acknowledgments
This work was supported by a 2-Year Research Grant of Pusan National University.
This study was approved by the institutional review board (IRB) of the Pusan National University Korean Medicine Hospital.