A Study of the Effect on Obesity and dyslipidemia in Kidney-hypofunction Animal Model Induced by Unilateral Ureteral Obstruction
Article information
Abstract
Objectives
The objective of this study is to develop a new animal model with Kidney-hypofunction for Sasang Constitutional Medicine, especially for partial Soyangin(one of four constitution which has good digestive function and poor renal function) by Unilateral Ureteral Obstruction, and to estimate the factor related to obesity, dyslipidemia, and metabolic syndrome.
Methods
The C57BL/6J mice were divided into 3 groups: normal group, high fat diet(HFD) control group, and HFD group with Unilateral Ureteral Obstruction(UUO). Then, the HFD control group and the experimental group were fed with high fat diet for 6 weeks. Food intake and body weight were measured at regular time by week. After the final experiment, blood was gathered for bloodchemical examination and organs(liver, fatty tissue) were remoed, weighted, and mRNA was analyzed with real-time PCR.
Results
The weight growth rate with High fat diet went down by 8.35% in experimental group and had similar FER with the normal group, while HFD control group had higher weight growth rate and FER than any other groups. Also The experimental group had lower triglyceride and LDL cholesterol rate and higher glucose rate in serum. and in mRNA expression, GLUT-9, the protein related to excretion of uric acid and metabolic syndrome, expressed lower rate than that of HFD control group. and IL-6, a kind of cytokine related to obesity and metabolic syndrome, expressed more than HFD control group.
Conclusions
It was found that Kidney-hypofunction animal-experimental model is susceptible to metabolic syndrome.
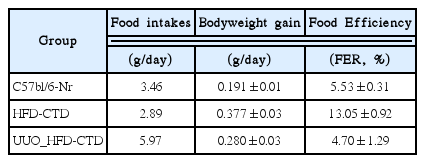
Body weight change in HFD-induced obese mice, and -renal cortex of each study group(UUO: unilateral ureteral obstruction) obese mice.
C57bl/6J-Nr: C57bl/6J normal group (n=5) HFD-CTL: High Fat Diet-Negative Control (n=5)
UUO_HFD-CTL: High Fat Diet group with unilateral ureteral obstruction (n=5)
Food efficiency ratio (FER, %) in HFD-induced obese mice, and -renal cortex of each study group(UUO: unilateral ureteral obstruction) obese mice.
C57bl/6J-Nr: C57bl/6J normal group (n=5) HFD-CTL: High Fat Diet-Negative Control (n=5)
UUO_HFD-CTL: High Fat Diet group with unilateral ureteral obstruction (n=5)
AST, ALT level in serum of HFD-induced obese mice, and -renal cortex of each study group(UUO: unilateral ureteral obstruction) obese mice.
C57bl/6J-Nr: C57bl/6J normal group (n=5) HFD-CTL: High Fat Diet-Negative Control (n=5)
UUO_HFD-CTL: High Fat Diet group with unilateral ureteral obstruction (n=5)
Creatine level in serum of HFD-induced obese mice, and -renal cortex of each study group(UUO: unilateral ureteral obstruction) obese mice.
C57bl/6J-Nr: C57bl/6J normal group (n=5) HFD-CTL: High Fat Diet-Negative Control (n=5) UUO_HFD-CTL: High Fat Diet group with unilateral ureteral obstruction (n=5)
Total Cholesterol level in serum of HFD-induced obese mice, and -renal cortex of each study group(UUO: unilateral ureteral obstruction) obese mice.
C57bl/6J-Nr: C57bl/6J normal group (n=5) HFD-CTL: High Fat Diet-Negative Control (n=5) UUO_HFD-CTL: High Fat Diet group with unilateral ureteral obstruction (n=5)
HDL and LDL Cholesterol level in serum of HFD-induced obese mice, and -renal cortex of each study group(UUO: unilateral ureteral obstruction) obese mice.
C57bl/6J-Nr: C57bl/6J normal group (n=5) HFD-CTL: High Fat Diet-Negative Control (n=5) UUO_HFD-CTL: High Fat Diet group with unilateral ureteral obstruction (n=5)
Glucose level in serum of HFD-induced obese mice, and -renal cortex of each study group(UUO: unilateral ureteral obstruction) obese mice.
C57bl/6J-Nr: C57bl/6J normal group (n=5) HFD-CTL: High Fat Diet-Negative Control (n=5) UUO_HFD-CTL: High Fat Diet group with unilateral ureteral obstruction (n=5)
Abdominal subcutaneous fat and Epididymal adipose tissue weight in HFD-induced obese mice, and -renal cortex of each study group(UUO: unilateral ureteral obstruction) obese mice.
C57bl/6J-Nr: C57bl/6J normal group (n=5) HFD-CTL: High Fat Diet-Negative Control (n=5) UUO_HFD-CTL: High Fat Diet group with unilateral ureteral obstruction (n=5)
Liver weight in HFD-induced obese mice, and -renal cortex of each study group(UUO: unilateral ureteral obstruction) obese mice.
C57bl/6J-Nr: C57bl/6J normal group (n=5) HFD-CTL: High Fat Diet-Negative Control (n=5) UUO_HFD-CTL: High Fat Diet group with unilateral ureteral obstruction (n=5)
mRNA expression of GLUT-9, IL-6, COX-2 were measured with Real Time-PCR analysis.
C57bl/6J: C57bl/6J normal group (n=5)
HFD-CTL: High Fat Diet-Negative Control (n=5)
UUO_HFD-CTL: High Fat Diet group with unilateral ureteral obstruction (n=5)