Development of Standardized Predictive Models for Traditional Korean Medical Diagnostic Pattern Identification in Stroke Subjects: A Hospital-based Multi-center Trial
Article information
Abstract
Objectives
To develop a standardized diagnostic pattern identification equation for stroke patients, our group conducted a study to derive the predictive logistic equations. However, the sample size was relatively small. In the current study, we aimed to derive new predictive logistic equations for each diagnostic pattern using an expanded number of subjects.
Methods
This study was a hospital-based multi-center trial recruited stroke patients within 30 days of symptom onset. Patients’ general information, and the variables related to diagnostic pattern identification were measured. The diagnostic pattern of each patient was identified independently by two Korean Medicine Doctors. To derive a predictive model for pattern identification, binary logistic regression analysis was applied.
Results
Among the 1,251 patients, 385 patients (30.8%) had the Fire Heat Pattern, 460 patients (36.8%) the Phlegm Dampness Pattern, 212 patients (16.9%) the Qi Deficiency Pattern, and 194 patients (15.5%) the Yin Deficiency Pattern. After the regression analysis, the predictive logistic equations for each pattern were determined.
Conclusion
The predictive equations for Fire Heat, Phlegm Dampness, Qi Deficiency, and Yin Deficiency would be useful to determine individual stroke patients’ pattern identification in the clinical setting. However, further studies using objective measurements are necessary to validate these data.
Introduction
Stroke can be fatal or lead to irreversible neurological deficits such as hemiplegia, problems with speech or comprehension, or sense dysfunction1). To prevent occurrence of irreversible neurological deficits and secondary stroke, several acute stroke management therapies are employed, and include treatment with recombinant tissue plasminogen activator (rtPA), a protein involved in the breakdown of blood clots2,3), antiplatelet agents4) in ischemic stroke and antihypertensive therapy5,6), aspiration surgery6) in hemorrhagic stroke. However, these therapies have drawbacks, such as the short time window for administration of rtPA and the adverse effects, including bleeding, induced by rtPA or antiplatelets2–4).
The alternative and complementary medicine therapies have received recent attention to make up for those limitations of western medicine7). Previous studies have suggested that therapies such as herbal medicine, acupuncture, electroacupuncture, moxibustion and pharmacoacupuncture are effective in various fields of stroke therapy such as acute of small vessel occlusion (SVO)11,12), post-stroke spasticity13), motor recovery after stroke14–16), post-stroke aphasia17) and shoulder pain induced by hemiplegia18).
Pattern-identification is a unique diagnostic system in Korean Medicine (KM), Traditional Chinese Medicine and Japanese Kampo medicine. It is an approach to investigate the causative factors, location, and prognosis of diseases according to correlation of all four examinations such as inspection, inquiry, listening and smelling examination, and palpation19). According to these pattern-identifications, future therapeutic plans are set. Therefore, proper diagnostic pattern-identification is essential to promote the beneficial effects of therapies. To enhance the objectivity of diagnostic pattern-identification, several studies have been conducted in the East Asian region20–27). However, most of these studies did not suggest objective coefficient values that could indicate the importance of variables for determining a diagnostic pattern. Furthermore, most21–26) were based on a very small sample size. Most importantly, the subjects of most of these studies20,22–25) were not stroke subjects and therefore the results could not be used to apply therapies for stroke management.
From 2005 to 2011, the Committee of Korean standard differentiation of the symptoms and signs for the stroke had been worked in Korea. In this work, the Committee suggested four types of stroke pattern identification (the Fire Heat Pattern, the Phlegm Dampness Pattern, the Qi Deficiency Pattern, and the Yin Deficiency Pattern) with agreement of experts28–30). We conducted binary logistic regression analysis to identify the variables that affected these four pattern-identifications and derive the predictive logistic equations for stroke subjects in 2011 to develop a standardized diagnostic pattern-identification equation for stroke subjects31). Where, the predictive logistic equations for the Fire Heat Pattern, the Phlegm Dampness Pattern, the Qi Deficiency Pattern, and the Yin Deficiency Pattern were suggested. However, the sample size of the previous study was relatively small.
In the current study, we aimed to derive new predictive logistic equations for each diagnostic pattern using an expanded number of subjects.
Materials and Methods
1. Subjects
This study was a hospital-based multi-center trial in patients from Korean Medicine university hospitals in the national capital region including Seoul Metropolitan City, and Incheon Metropolitan City as follows: Kyung Hee University Korean Medicine Hospital (Seoul), Kyung Hee University Korean Medicine Hospital at Gangdong (Seoul), and Gil Oriental Medical Hospital of Gacheon University (Incheon). The Institutional Review Board (IRB) approved this study (KOMC IRB 2011-02, KHNMCOHIRB-2012-003, and KWOMH IRB 2006-101).
Subjects with ischemic and hemorrhagic stroke who met International Statistical Classification of Diseases and Related Health Problems 10th revision code I63 and I61 within 30 days of symptom onset, confirmed by computerized tomography or magnetic resonance imaging were included. Subjects with traumatic stroke such as those with subarachnoid, subdural, and epidural hemorrhage were excluded. Subjects had been enrolled consecutively between April 2007 and December 2012. If there are patients who experienced two or more stroke attack during follow-up period, we only use the data which were obtained in the first admission time. Informed consent was obtained from all study subjects or protectors after a full explanation of the study.
2. Measured Variables
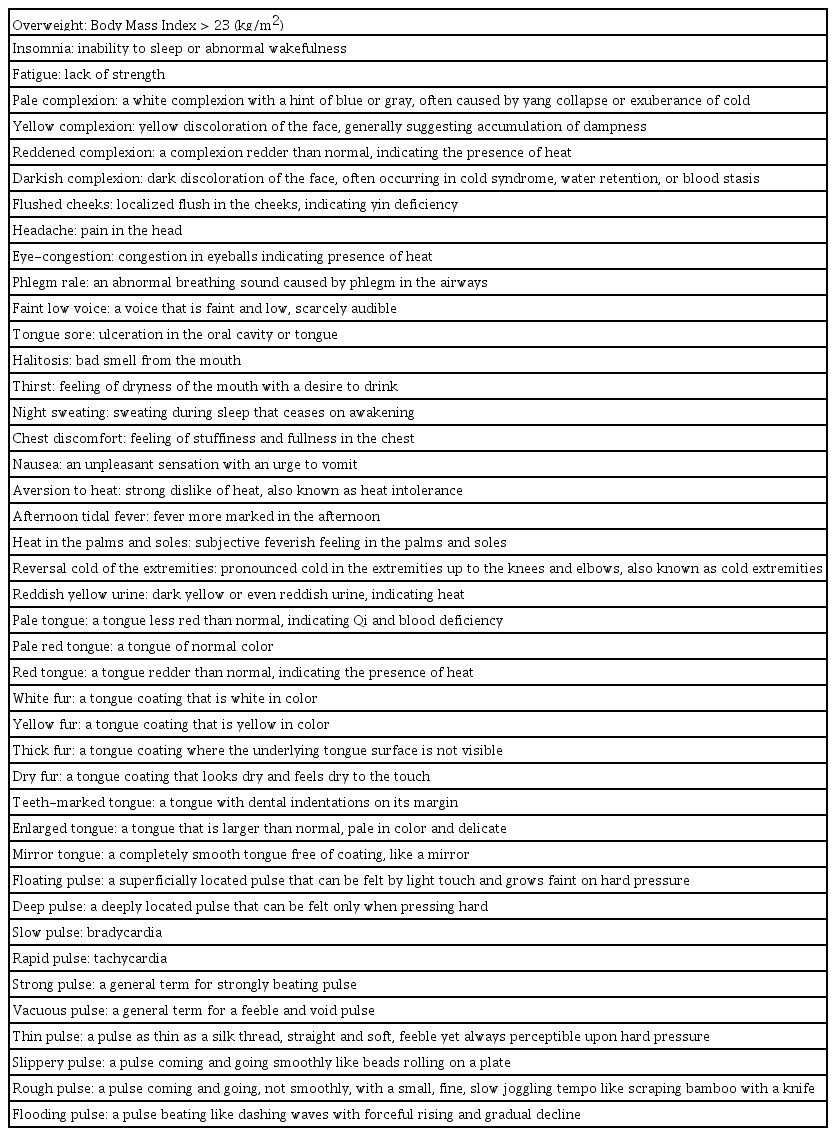
Subjects’ general information including medical history including stroke risk factors, the Trial of ORG 10172 in Acute Stroke Treatment (TOAST)32,33) classification of the stroke, as well as the variables related to diagnostic pattern–identification (Appendix 1) were measured. All the variables in this study are binary pattern; yes or no. The translation of these medical terms into English was based on the guideline suggested by the World Health Organization (WHO)34).
These subjects’ data were collected using Case Report Forms (CRFs) and Standard Operation Procedures (SOPs) made by the expert committee of the Korean Institute of Oriental Medicine (KIOM)28–30,35,36) were used. These CRFs and SOPs are the same format used in previous study31). These procedures were independently conducted without discussion among KMDs (Korean Medicine Doctors). One KMD recorded CRFs and decided KM diagnostic pattern–identification after examination. Another KMD just decided KM diagnostic pattern-identification after examination.
3. Determination of Pattern Identification and a New Diagnostic Pattern Identification Equation
The diagnostic pattern of each subject was identified independently by two KMDs, each of whom belonged to one of the study hospital and had 3 years or more clinical experience with stroke management. The categories of identified pattern were the Fire Heat, the Phlegm Dampness, the Qi Deficiency, and the Yin Deficiency Pattern. These categories of identified pattern were suggested by KIOM (Korea Institute of Oriental Medicine)28–30,35) and used in previous study31). The pattern of each subject was confirmed if the two doctors had the same opinion. Cases where the two doctors had different opinions comprised an unclassified group.
Binary logistic regression was used to detect significant variables which affect the Pattern–Identification decision. To remove the variables that had no statistical significance step-by-step, a backward method was used until a logistic equation composed of absolutely significant variables was reached, and each retained variable considered as an independent factor for the predictive model. Fire Heat, Phlegm Dampness, Qi Deficiency, and Yin Deficiency were studied. The derived logistic equation was as follows: log (P/1-P) = β0+β1Χ1+β2Χ2+⋯+βnΧn. In this equation, Χs are independent variables, βs are regression coefficients, and P is the calculated probability of the pattern-identification. According to the β coefficient, there would be positively quantified or negatively quantified variables, i.e., if a subject had more positives, the probability of the pattern-identification would increase, whereas if there were more negatives, the probability of non-pattern-identification would increase. The statistical analysis was performed using SPSS for Windows, version 16.0 (SPSS Inc., Chicago, Illinois, USA).
Results
1. General Characteristics of Each Pattern Identification
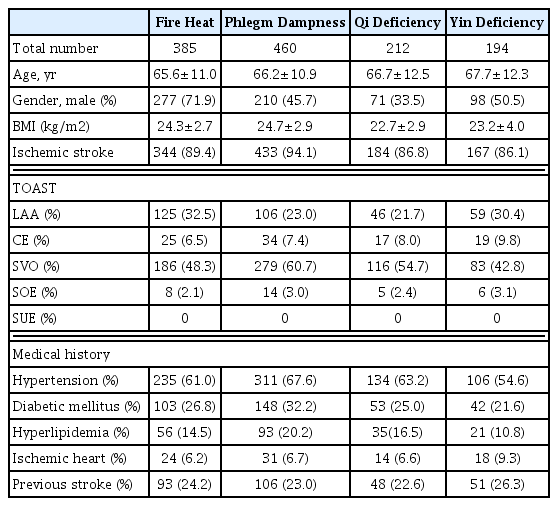
A total of 1,972 stroke patients were recruited. Of these, 721 could not be classified as having a certain pattern because the diagnoses of the two doctors differed. These patients were excluded from the analyses. Among the remaining 1,251 patients, 385 patients (30.8%) had the Fire Heat Pattern, 460 patients (36.8%) the Phlegm Dampness Pattern, 212 patients (16.9%) the Qi Deficiency Pattern, and 194 patients (15.5%) the Yin Deficiency Pattern. The Fire Heat Pattern was more common among men, and the Phlegm Dampness Pattern was most common among patients who exhibited more variables related to the metabolic syndrome (hypertension, diabetic mellitus, and dyslipidemia). Previous ischemic heart disease was exhibited most commonly under the Yin Deficiency Pattern. Most (86.1~94.1%) subjects had ischemic stroke of all subtypes. Among the TOAST subtype classifications32,33), all four diagnostic patterns were similarly represented, with SVO being the most common (Table 1). Herein, only descriptive statistics were applied; comparative statistical analysis was not performed because of the lack of balance in the sample sizes of the pattern groups.
2. Retained Significant Symptoms for Fire Heat Pattern and Identification of Fire Heat Diagnostic Pattern Equation
There were 385 patients (30.8% of the total identified patients) in whom two doctors identified Fire Heat Pattern. Teeth marked tongue, vacuous pulse, halitosis, thirst, and heat in the palms and soles showed relatively high significance in the first analysis, but were removed as the backward method progressed. Finally, overweight, fatigue, yellow complexion, reddened complexion, darkish complexion, tongue sore, aversion to heat, reversal cold of the extremities, reddish yellow urine, pale tongue, yellow fur, thick fur, dry fur, deep pulse, slow pulse, strong pulse, thin pulse, slippery pulse, and flooding pulse all showed highly statistically significant correlations with the Fire Heat pattern and were retained in the equation.
Thus, we derived the predictive logistic equation:
3. Retained Significant Symptoms for Phlegm Dampness Pattern and Identification of Phlegm Dampness Diagnostic Pattern Equation
There were 460 patients (36.8% of the total identified patients) in whom two doctors identified Phlegm Dampness Pattern. All of the assessed variables were included in the first logistic regression analysis. Yellowish complexion, reddened complexion, flushed cheeks, nausea, phlegm rale, halitosis, chest discomfort, reddish yellow urine, red tongue, yellow fur, white fur, deep pulse, vacuous pulse, and aversion to heatexhibited relatively high significance at the first analysis, but were removed as the backward method progressed. Ultimately, overweight, darkish complexion, faint low voice, night sweating, pale tongue, dry fur, slow pulse, rapid pulse, thin pulse, slippery pulse, and flooding pulse all showed high statistical significance and were retained in the equation.
Thus, we derived the predictive logistic equation:
4. Retained Significant Symptoms for Qi Deficiency Pattern and Identification of Qi Deficiency Diagnostic Pattern Equation
There were 212 patients (16.9% of the total identified patients) in whom two doctors identified Qi Deficiency Pattern. All of the assessed variables were included in the first logistic regression analysis. Headache, red tongue, reddish yellow urine, chest discomfort, heat in the palms and soles, and strong pulse showed relatively high significance at the first analysis, but were removed as the backward method progressed. As a result, overweight, insomnia, fatigue, pale complexion, reddened complexion, faint low voice, tongue sore, halitosis, thirst, aversion to heat, reversal cold of the extrimities, yellow fur, thick fur, dry fur, teeth marked tongue, slow pulse, rapid pulse, vascuous pulse, thin pulse, and slippery pulse all showed high statistical significance and were retained in the equation.
Thus, we derived the predictive logistic equation:
5. Retained Significant Symptoms for Yin Deficiency Pattern and Identification of Yin Deficiency Diagnostic Pattern Equation
There were 194 patients (15.5% of the total identified patients) in whom two doctors identified Yin Deficiency Pattern. All of the assessed variables were included in the first logistic regression analysis. Fatigue, pale complexion, tongue sore, and red tongue showed relatively high significance at the first analysis, but were removed as the backward method progressed. As a result, overweight, flushed cheeks, faint low voice, halitosis, afternoon tidal fever, night sweating, pale tongue, yellow fur, dry fur, floating pulse, deep pulse, slow pulse, strong pulse, thin pulse, slippery pulse, and flooding pulse all showed high statistical significance and were retained in the equation.
Thus, we derived the predictive logistic equation:
Discussion
The present study was designed to increase the accuracy and reliability of the Traditional Korean Medical Diagnostic Pattern-identification logistic equation model, which was first reported in 201131).
There are two issues at point. First, the information directly obtained by KMDs such as inspection, tongue diagnosis, and pulse diagnosis play more important roles to make the predictive equation than the subjects’ subjective complaints. Based on these data, we could know that KMDs are more concerned with the data obtained by physical examination than the data obtained by medical interview in the process of the pattern identification decision. Second, overweight might be also an important variable in determining diagnostic pattern. In practice, overweight was included in every type of equation. Therefore, body shape could also be a key point in the process of pattern identification decision.
The characteristics of each diagnostic Pattern–Identification derived from this study are as follows. The excessive patterns such as Fire Heat and the Phlegm Dampness Pattern have positively quantified variables in higher proportion than other patterns. Therefore, determining these two patterns could be an inclusive pattern. On the other hand, the deficiency pattern such as Qi and Yin Deficiency Patterns revealed an exclusive pattern composed of many negatively quantified variables.
In this study, we did not investigate the blood stasis, one of the pattern identification types that has been thought to be the main pattern identification of the stroke. The reason for this is as follows. In version 1 of KIOM’s study, which established the categories of pattern identification used in the present study, five pattern identification types were included (including blood stasis). However, blood stasis was found in only 24 (2.8%) out of 859 patients in investigation of version 237). Different clinical circumstances in Korea and China had been noted for this result. In Korea, a medical classic, Dongeuibogam has been set as the basic text. Unlike Chinese literature, Doneuibogam didn’t record blood stasis as one of the pattern identification of the stroke37). Therefore, blood stasis type was excluded in version 330), and we did not investigate blood stasis according to version 3.
There are some limitations in the present study as well. Inspection, tongue and pulse diagnosis were obliged to rely on the KMDs’ subjective perception. To overcome this, objective measurements should be developed and suggested. Because this is not a community-based study, our results could not be generalized for Korean people. Finally, in this study, we excluded cases which the decision on pattern identification of two experts was different considering the difficulty of statistical processing. As a result, we could not evaluate the situation which two or more pattern identification types were mixed. Future studies need other statistical processing methods that can reflect the situation in which two or more pattern identification are mixed.
The strengths of this study are as follows. First, new predictive logistic diagnostic pattern equations including more significant variables and based on larger samples are coming up. Second, coefficients in diagnostic patterns as derived by binary logistic regression analysis are suggested. Among study groups of traditional medicine in East Asia, there have been several studies to suggest the significant variables for the determination of diagnostic patterns. In Japan, several standardized questionnaires have been suggested: OKETSU (blood stasis)20), Qi Deficiency, Qi movement Stagnation27), Phlegm Dampness, and Cold-Heat Pattern-identification. In these questionnaires, coefficients for each value were suggested. However, only the OKETSU questionnaire by Terasawa et al20) and the Qi movement Stagnation questionnaire by Oketsu27) clearly stated the methodology and development process. In China, there have been similar attempts at standardization of diagnostic pattern-identification. The standard form of pattern-identification for stroke subjects was suggested in 199421). However, the form of this suggestion is only the list of symptoms. There was no coefficient that could reveal the importance of each symptom in each pattern. In Korea, similar suggestions exist. Kim et al suggested a questionnaire for the Heat Pattern22 and Park et al suggested a questionnaire for the Phelgm Dampness Pattern25). However, both of them were developed using the Delphi method from KMD clinicians. In 2012, Lee et al established five stroke patterns from the traditional Korean Medical literature and extracted 117 indicators required for diagnosis. These indicators were evaluated by a field test and verified by an expert committee however, they did not suggest coefficients26). In this study, binary logistic regression analysis was applied to derive significant variables for the determination of each diagnostic pattern in order to overcome the limitations of the studies described above.
In this study, standardization of the Traditional Korean Medical Pattern-identification in stroke subjects was intended. After the regression analysis, the predictive logistic equations for Fire Heat, Phlegm Dampness, Qi Deficiency, and Yin Deficiency pattern were determined. These criteria would be useful to determine individual stroke subjects’ pattern-identification in the clinical setting. Furthermore, we think the result of this study could be able to be a supportive teaching material for improving Traditional Korean Medicine Doctors’ clinical ability for pattern identification.
Acknowledgments
Aknowledgements
This work was supported by a Grant from the Korean Institute of Oriental Medicine (K09200). This paper is based on Seungwon Kwon’s doctoral dissertation.
Notes
Competing Interests
The authors declare that they have no competing interests.