References
1. Urwin M, Symmons D, Allison T, Brammah T, Busby H, Roxby M, et al. Estimating the burden of musculoskeletal disorders in the community: The comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Ann Rheum Dis 1998;57(11):649–55.
2. Shanahan EM, Sladek R. Shoulder pain at the workplace. Best Pract Res Clin Rheumatol 2011;25(1):59–68.
3. Widar M, Ahlström G, Ek AC. Health-related quality of life in persons with long-term pain after a stroke. J Clin Nurs 2004;13(4):497–505.
4. Kim SH. Orthopedic disease and sports medicine in shoulder joint. J Korean Med Assoc 2011;54(7):705–14.
5. Ombregt L. A System of Orthopaedic Medicine 3rd edth ed. Seoul: Hanmi medical publishing Co; 2017. p. 376.
6. Lee H. Differential diagnosis of common shoulder pain. J Korean Med Assoc 2014;57(8):653–60.
7. Han TR, Bang MS, Chung SG. Rehabilitation medicine 6th edth ed. Seoul: Koonja Publishing; 2019. p. 1382.
8. Gamble GE, Barberan E, Laasch HU, Bowsher D, Tyrrell PJ, Jones AKP. Poststroke shoulder pain: A prospective study of the association and risk factors in 152 patients from a consecutive cohort of 205 patients presenting with stroke. Eur J Pain 2002;6(6):467–74.
9. Langhorne P, Stott DJ, Robertson L, MacDonald J, Jones L, McAlpine C, et al. Medical Complications After Stroke. Stroke 2000;31(6):1223–9.
10. Korea Institute of Oriental Medicine. Shoulder Pain in adults – Korean Medicine Clinical Pracise Guideline 1st edth ed. Seoul: Elsevier Korea L.L.C; 2015. p. 222.
11. Green S, Buchbinder R, Hetrick SE. Acupuncture for shoulder pain. Cochrane Database Syst Rev 2005;(2)
12. Kim SY, Park JE, Lee YJ, Seo HJ, Sheen SS, Hahn S, et al. Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J Clin Epidemiol 2013;66(4):408–414.
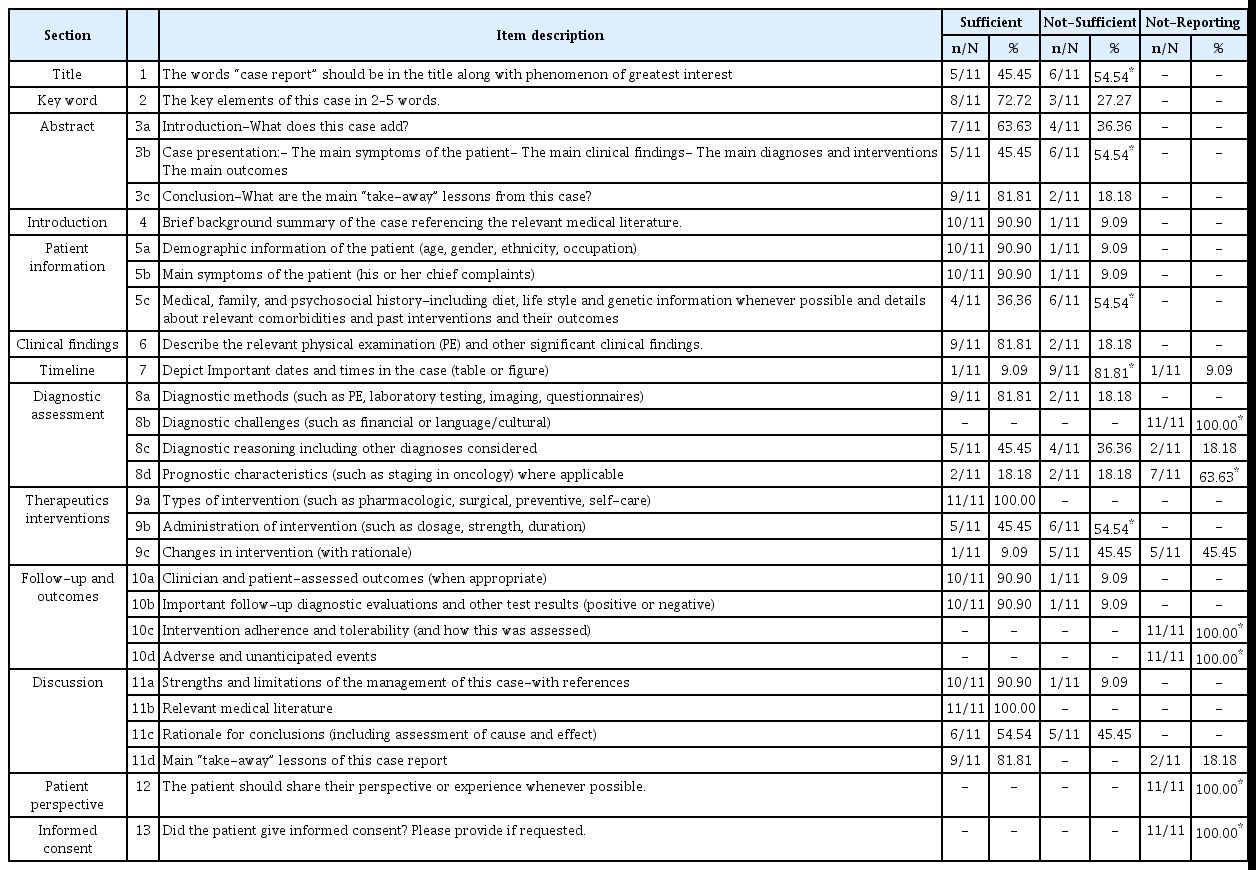
13. Riley DS, Barber MS, Kienle GS, Aronson JK, von Schoen-Angerer T, Tugwell P, et al. CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol 2017;89:218–235.
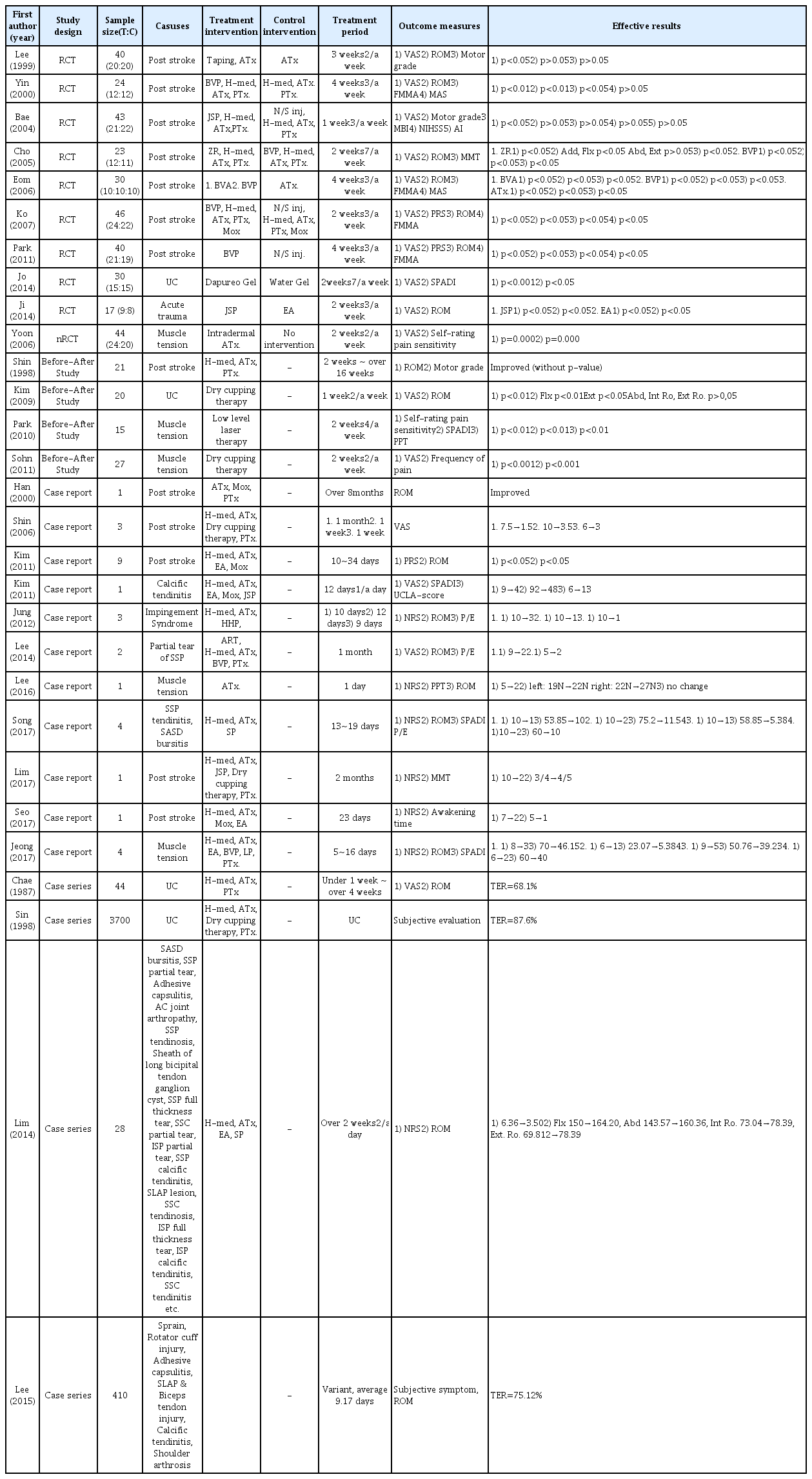
14. Eom JY, Won SH, Kwon KR, Sook LH. Comparative study of Acupuncture, Bee Venom Acupuncture and Bee Venom Herbal Acupuncture on the treatment of Post-stroke Hemiplegic Shoulder Pain. J Pharmacopuncture 2006;9(1):139–54.
15. Ko CN, Min IK, Park SW, Jung WS, Kwan MS, Park JM, et al. Effectiveness of Bee Venom Acupuncture on Shoulder Pain after Stroke. J Korean Med 2007;28(1):11–24.
16. Ji MJ, Lim SC, Kim JS, Lee HJ, Lee YK. The Comparative Study on Effect of Jungsongouhyul Phamacopuncture and Electroacupuncture in Patients with Acute Traumatic Shoulder Pain. J Acupunct Res 2014;31(4):205–11.
17. Sin WU, Kim SH, Song HJ. Case report of hyperpigmentation in 3700 case of shoulder pain patients traeted with cupping therapy. J Haehwa Med 1998;6(2):303–11.
18. Lee JE, Oh MS. The Retrospective Review of 410 Shoulder Pain Inpatients in Korean Medicine Hospital. J Korean Med Rehabil 2015;25(2):155–73.
19. Chae WS, Lee JG, Lee BR. Clinical Study on 44 shoulder Pain Patients. J Korean Med 1987;8(2):49–55.
20. Lim SJ, Jun JY, Lee CW, Kim HS, Kim HS, Bae YH, et al. Clinical Characteristics and Treatment Effects of Shoulder Pain Patients Admitted to a Korean Medicine Hospital Based on MRI Findings. J Acupunct Res 2014;31(4):109–19.
21. Kim JH, Kwak HY, Jung KY, Seon JI, Lee UI, Nam DW, et al. A Case Report on the Effect of Electroacupuncture at LI15 and TE14 for the Treatment of Shoulder Pain in Post-stroke Hemiplegia Patients. J Acupunct Res 2011;28(6):159–67.
22. Song KC, Seo JY, Song SB, Cho MU, Choi BS, Ryu WH, et al. A Case Report on the improvement of Range of Motion and Pain Relief for Patients Diagnosed with Supraspinatus Tendinosis, Subacromial Bursitis and Subdeltoid Bursitis treated with Megadose Shinbaro Pharmacopuncture. J Haehwa Med 2017;26(1):73–80.
23. Jeong SJ, Jin JY, Kwak MK, Kim SA, Wei TS. Four Cases of Shoulder Pain Treated by Ligamentum Pharmacopuncture on Kyonu (LI15), Gyeollyo(TE14), Geogol(LI16) and Nosu(SI10). Korean J Acupunct 2017;34(4):271–6.
24. Jung YG, Kim MY, Kim JS, Choi Y Il, Choi HS, Cho TY. A Case Report of Prescribing Geumchuldodam-tang for the Three Patients with Shoulder Impingement Syndrome. J Korea CHUNA Man Med Spine Nerves 2012;7(1):85–94.
25. Shin WY, Hyun JO, Choi EY, Kang AM, Kim YH, Jo EY, et al. 3 Case Reports of Cheongungkyeoji-tang for Post-stroke Patients with Shoulder Pain. J Intern Korean Med 2006;27(4):936–44.
26. Lee SJ, Park JH, Nam SH, Kang JH. Two Clinical Cases of Active Release Technique with Koeran Medicine Treatment for Supraspinatus Tendon Partial Tear. J Korea CHUNA Man Med spine nerves 2014;9(1):89–101.
27. Lee HJ, Lee NH, Son CG, Cho JH. Acupuncture Stimulation on LR3 Reduced Shoulder Pain Caused by Upper Trapezius Rigidity. A Case Report. J Haehwa Med 2016;25(1):63–9.
28. Sohn D, Yoon HM, Jung HM. The Effects of Dry Cupping Therapy on the Shoulder Pain and Fatigue of Nurses. J Pharmacopuncture 2011;14(2):25–36.
29. Park KM, Lee GJ, Song YK, Lim HH. The Clinical Effects of Low Level Laser Therapy on Shoulder Pain. J Korean Med Rehabil 2010;20(1):183–92.
30. Han MG, Heo SY. The study of rehabilitational treatment on shoulder pain in hemiplegic stroke patients. J Jeahan Orient Med Acad 2000;5(1):43–53.
31. Kim NH, Jang HJ, Kim JH, Hwang DS, Bock JJ. A Clinical Study on the Case of Right Shoulder Pain occurred in Calclfic tendinitis. J Orient Med Thermol 2011;9(1):37–43.
32. Seo HJ, Cho JH, Bae GE, Choi JY, Shim SH, Han CW, et al. A Case Report of a Cerebral Infarction Patient with Shoulder Pain Using Korean Medical Treatment. J Soc Stroke Korean Med 2017;18(1):87–96.
33. Lee SH, Chung SH, Lee JS, Kim SS, Dae SH. The Effect of Scapular Girdle Taping on Hemiplegic Shoulder Pain: A Clinical Study. J Korean Med 1999;20(3):115–26.
34. Jo SJ, Choi YD, Jang JT, Kim KS, Lee SD. A Randomized Controlled Clinical Trial of Topical Herbal Gel Treatment for Chronic Shoulder Pain. J Acupunct Res 2014;31(4):1–9.
35. Park JA, Lee CH, Kwon GS, Lee KA, Jang KJ. The Effects of Sweet Bee Venom Pharmacopuncture on the Post-stroke Hemiplegic Shoulder Pain. J Acupunct Res 2011;28(4):37–47.
36. Yin CS, Nam SS, Kim YS, Dong LJ, Kim CH, Koh HK. Effects of Honeybee Venom Acupuncture Therapy on the Poststroke Hemiplegic Shoulder Pain. J Pharmacopuncture 2000;3(2):213–32.
37. Bae HH, Park YC. Effectiveness of Jungsongouhyul Pharmacopuncture Simultaneous Treatment on Poststroke Shoulder Pain. J Pharmacopuncture 2004;7(1):77–86.
38. Cho SW, Go KH, Nam JH, Kim MS, Lee SY, Lee IS, et al. The Effectiveness of Zingiberis Rhizoma Herbal Acupuncture Therapy and Bee Venom Herbal Acupuncture Therapy on the Poststroke Hemiplegic Shoulder Pain. J Korean Med Rehabil 2005;15(4):77–87.
39. Yoon HM, Kim JH, Lee JW. The Effect of Intradermal Acupuncture Therapy at Kyeonjeong, Cheonryo and Kokji on the Shoulder Pain. J Acupunct Res 2006;23(5):155–65.
40. Shin BC, Kwon YD, Song YS. Radiological clinical study on shoulder subluxation due to post-stroke paralysis. J Korean Med Rehabil 1998;8(2):383–403.
41. Kim HS. The effect of dry cupping therapy on the pain relief and ROM changes of the shoulder Soeul: Graduate School of Engineering, Konkuk University; 2009. p. 53.
42. Lee GY, Jo HG, Seol JU, Kim SA. A Review of the Pain and Function Assessment Instruments for Shoulder Disease Patients in Korean Medicine Clinical Studies Published in South Korea. J Korean Med Rehabil 2018;28(1):33–51.
43. Kim HW, Kim SS, Park SW, Kim EK, Lee GH, Lee GM. A Systematic Review of Randomized Controlled Trials on Acupuncture Treatment for Shoulder Pain. J Acupunct Res 2010;27(4):67–84.
44. Choi H-M, Han S-Y, Hwang D-R, Kang J-H. Acupuncture Treatment for Rotator Cuff Disorder: A Systematic Review. J Korean Med Rehabil 2018;28(4):11–20.
45. Choi SY. Evaluation of the Quality of Case Reports from the Journal of Korean Medicine Based on the CARE Guidelines 2020;41(May):122–36.
46. Lee HL, Kim JH, Lee MS, Lee JA. Evaluation of the Quality of the Case Reports from the Journal of Pediatrics of Korean Medicine Based on the CARE Guidelines. J Korean Med 2018;32(3):131–40.
47. Kim JH, Lim LH, Lee JA, Lee MS. Assesment of The Quality of Reporting in Case Reports in Journal of Sasang Constitutional Medicine from Year 2015 to 2018: Using CARE Guidelines. 2018;30(2):28–41.
48. Lee HS, Lee J, Han JH, Chae H. Evaluation of the Quality of Case Reports in Journal of Oriental Neuropsychiatry Using CARES Guideline. 2019;30(2):59–69.
49. Nam EY, Park JY. Evaluation of the Quality of the Case Reports from the Journal of Obstetrics and Gynecology of Korean Medicine Based on the CARE Guidelines. 2019;32(2):71–86.
50. Ahn JH, Ko JH, Kim SY, Kim SJ, Bae JH, Yoon YJ, et al. Evaluation of Adherence to the CARE (CAse REport) Guidelines of Case Reports in the Journal of Korean Medicine Rehabilitation. J Korean Med Rehabil 2019;29(3):75–85.