Effect of Nokyongdaebo-tang on chronic anemia in Taeumin wiwansuhan-pyohan disease (胃脘受寒表寒病) patient: a case report
Article information
Abstract
Objectives
The present study reports a case of chronic anemia patient who was significantly improved after taking Nokyongdaebo-tang (NYDBT)
Methods
A 48-year-old male patient diagnosed with iron deficiency anemia (IDA) visited the Daejeon Korean medicine Hospital of Daejeon University on June 2018. The patient was treated with Korean medicine for 23 months including acupuncture, herbal medicine and Sasang constitutional medicine prescription. Improvement of anemia was assessed by changes of Hemoglobin value. Laboratory analysis was used to evaluate the safety of treatment.
Results
Chronic anemia has significantly improved since taking NYDBT on 9 days (2019.12.09–2019.12.17). The Hb value has been maintained in the normal range since it first entered the normal range on January 18, 2020. The patient had become transfusion-free and this condition persisted for 6 months after stopping the transfusion.
Conclusion
This case demonstrates the therapeutic potential of Sasang constitutional medicine for chronic anemia as a personalized medicine.
Introduction
Anemia is defined as a reduction in number of red blood cells (RBCs) or less than the normal quantity of Hemoglobin (Hb) in the blood1). It is common problem encountered in primary care. A recent analysis of the prevalence of anemia in 195 countries estimated that its prevalence in 2015 was 33%, and the most common form was iron deficiency anemia (IDA) globally2).
The chief cause of IDA is chronic blood loss from the gastrointestinal tract. Beside identifying and treating the cause of gastrointestinal bleeding, patients with absolute iron deficiency (i.e., serum ferritin <100 ng/mL and transferrin saturation <20%) and anemia, should receive iron supplementation both to correct anemia and replenish iron stores3). RBC transfusion is discouraged in IDA in general, however adults presenting with extreme tiredness, at risk of cardiovascular instability or showing signs of heart failure or myocardial ischemia due to the severity of anemia (usually transfusion Hb <8.0 g/dL) should promptly receive transfusion to correct hypoxia and to return Hb to safe levels3,4).
This study reports the case of a chronic IDA patient who was improved by Sasang constitutional medical approach. The Sasang constitutional medicine is traditional Korean personalized medicine, which divides people into four types and suggests type-specific treatment for more effective and safe treatment. It is useful for the personalized application of traditional medicine such as acupuncture and medical herbs5).
Our patient had to receive RBC transfusion once or twice a month due to his recurrent episodes of severe anemia. But being treated by Traditional Korean medicine (TKM) including acupuncture and herbal medicine, his transfusion requirement was reduced. And after taking Nokyongdaebo-tang (NYDBT) in accordance with the diagnosis of Sasang constitutional medicine, he has maintained normal Hb values without transfusion for 6 months to date.
There have been many case reports that TKM treatment has improved anemia patients6–8), but this case is unique in that it has observed one patient for a relatively long period of time over two years and applied various TKM interventions, including acupuncture, herbal medicine and Sasang constitutional medicine. It has also been proven that the effect of treatment continues because the patient has been monitored for six months after treatment. We present outcome of this case as evidence of the utility of TKM for treating chronic anemia. Particularly, this case demonstrates the superiority of Sasang constitutional medicine as a personalized medicine. This study followed the Case Report Guideline (CARE guidelines)9) and was approved by the Institutional Review board of Daejeon University Korean medical hospital (DJDSKH-20-E-09).
Case report
1. Patient characteristics and medical history
A male patient, 48 years old, was diagnosed with IDA in 2014. Resistant to initial treatment with iron supplementation therapy, since May 2017 he required one to two transfusions per month so that by June 2018, he had received 76 units of RBCs. He complained of severe exhaustion symptoms associated with low Hb values. Because the lack of response to conventional treatments, he chose TKM as a cure for his disease. On June 6, 2018, the patient was attended a Korean medicine hospital as an outpatient for the first time.
Except being treated with pancreatitis in 2002, he has no special past medical history. And he has no family history of anemia or any other hematologic disorder. He used to drink alcohol (60g/day) every day from 1998 to 2002 and once a month from 2002.
2. Diagnosis and outcome evaluation
He was diagnosed with IDA in 2014 by laboratory tests including complete blood count (CBC), serum iron, serum ferritin and total iron-binding capacity (TIBC). Despite of upper and lower endoscopy, the underlying cause of iron deficiency was not determined. He had continued to take iron pills since diagnosis, but his Hb values were not responded to iron supplementation therapy. The reason why the Hb values had not been normalized was unexplained despite of medical examinations such as abdominal computer tomography (CT), repeated endoscopy, and bone marrow examination. He had a poor prognosis in that transfusion dependence is associated with decreased survival, higher rates of organ complications from iron overload10).
His Sasang constitutional type was classified as Taeumin based on both Questionnaires for the Sasang Constitution Classification II (QSCCII) and external appearance, voice, and personality trait of the patient. The symptom differentiation was Esophagus-Cold Lung-Dry (Wiwanhan-paejo) symptomatology of Esophagus cold-based exterior cold (Wiwansuhan-pyohan) disease in Taeumin. In depth classification, his symptom differentiation was Eumhyeol-mogal handa pattern, which was critical pattern of Wiwanhan-paejo symptomatology, according to his general symptoms such as absence of sweating, aversion to cold, shortness of breath, fearful throbbing and diarrhea. The symptoms of Eumhyeol-mogal handa pattern are described in Table 111).
CBC tests were used to assess the improvement of anemia. The transfusion requirement records were also used to evaluate the treatment. Laboratory results, including liver function tests, were used to assess the adverse effect of treatment.
2. Treatment and progress of symptoms
We divided periods into three based on the patient’s treatment and progress (Fig. 1).
There is a progressive reduction in transfusion requirement
Period I: The period from the first transfusion to the start of TKM treatment (2017.05.13–2018.06.06.06); Period II: The period from the start of TKM treatment to the start of treatment by NYDBT (2018.06.06–2019.12.09); Period III: The period from the start of treatment by NYDBT to date (2019.12.09–2020.05.02).
Period I is from the date the patient first received the transfusion until the start of TKM treatment (2017.05.13–2018.06.06.06). In Period I, he had received 76 units of packed RBCs for 13 months. Average RBC requirement per month in this period was 5.85 units (Fig. 1).
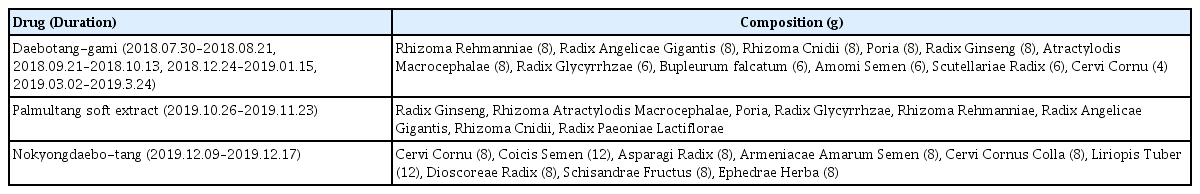
In period II, the patient started TKM treatment. He had received acupuncture treatment once a week and taken herbal medicine intermittently. Acupuncture treatment was performed for 15 minutes with 0.20 × 30 needles (DongBang Col, Seoul, Korea). We chose 4 acupoints (LU6, BL63, LI4, ST42), according to their meridian function toward the hematopoietic system and metabolic regulation based on the theory of TKM. And he was administered herbal drugs (Daebotang-gami and palmultang soft extract, Table 2) to improve his extreme deficiency syndrome. In this period, the patient’s subjective exhaustion symptom was improved, but the Hb values were not significantly increased. The patient had received 64 units of RBCs for 17 months so that average RBC requirement in this period was 3.76 units per month. Although the average transfusion requirement was reduced comparing to period I, it did not show a clear decreasing trend (Fig. 1) and the patient was still in transfusion-dependent state, so we assessed that the therapeutic effect was not sufficient.
Period III is from the start of NYDBT treatment to the latest follow-up date (2019.12.09–2020.05.02). On December 2019, we prescribed NYDBT to the patient by Sasang constitutional medicinal diagnosis. He had taken NYDBT (Table 2) three times a day for nine days. The patient’s Hb value began to increase after taking NYDBT. The Hb value has been maintained in the normal range since it first entered the normal range on 18 January 2020 and mean corpuscular volume (MCV) has been also normalized gradually (Fig. 2). The patient became transfusion-free after taking NYDBT (Fig. 1) and he also subjectively reported a notable improvement in exhaustion symptoms. In addition, his general symptoms (absence of sweating, aversion to cold, shortness of breath, fearful throbbing and diarrhea) which had made us to diagnose him as Taeumin Eumhyeol-mogal handa pattern were improved. His serum ferritin and TIBC tested on May 2, 2020 were 104 ng/ml and 320 ug/dl respectively, both of which were within the normal range.
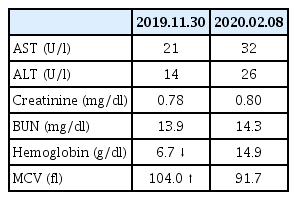
During the entire treatment period, the patient showed no adverse effects, including hepatotoxicity and nephrotoxicity (Table 3).
Discussion and conclusion
Anemia is common problem encountered in primary care and IDA is the most common anemia2). IDA can be treated by iron supplements but can easily induce digestive discomfort, especially constipation. In general, transfusion is discouraged in IDA, but in some cases transfusion can be considered to maintain the Hb to safe levels3,4). However transfusion dependence is associated with decreased survival, higher rates of comorbidities, immune responses, iron overload, and infections. In addition, quality of life (QOL) is negatively affected despite intermittent physiological hemoglobin levels achieved by RBC transfusion support10).
In this case report, the IDA patient had unexplained resistance to initial treatment with iron supplements and became transfusion-dependent requiring one to two transfusions per month. He chose TKM as complementary therapy for anemia. IDA is generally characterized as deficiency of qi and blood in TKM, so that supplement with qi and blood is general treatment of TKM for anemia12). Previous case studies reported that prescriptions which tonify qi and blood, such as Ickibohyoul-tang ga antler6), Ickibohyoul-tang, Samchulgunbi-tang7), and Guibitanggami8), had an effect on IDA patient.
At first, we prescribed herbal drugs Daebotang-gami and Palmultang soft extract, which are the typical prescription for deficiency syndrome, because we differentiated his anemia and anemia-related exhaustion symptom as syndrome of dual deficiency of qi and blood. Although the exhaustion symptom was improved and average transfusion requirement was reduced during the treatment, the therapeutic effect was insufficient considering that he was still dependent on blood transfusion. However NYDBT showed a clear effect on Hb value and it is obvious that transfusion-free state has been maintained for 6 months after treatment. Considering only the composition of the prescriptions (Table 2), the Daebotang-gami and Palmultang soft extract could be more effective for deficiency syndrome than NYDBT. However, NYDBT obviously improved not only Hb values but also his general symptoms associated with Taeumin pathological pattern. Therefore, the effect of NYDBT on anemia can be interpreted as a result of precise function of Sasang constitutional medical diagnosis.
NYDBT is classified as therapeutic agent of Taeumin Esophagus cold-based exterior cold (Wiwansuhan-pyohan) disease in Sasang constitutional medicine13). Several studies have been reported the bioactivities of NYDBT, which include neuroprotective activities to Alzheimer’s disease model14), antithrombotic activities15), hypolipidemic effects16), anti-aging activities17), and anti-oxidative effects18). Especially Kim’s study reported that NYDBT markedly and dose-dependently inhibited subacute hemorrhagic anemia related abnormal anemic signs in rats, suggesting the potential that NYDBT can be promising as a novel alternative hematopoietic and therapeutic agent for anemia19).
This case showed clear evidence of the utility of TKM for treating chronic anemia. The patient became transfusion-free and this state has been sustained for 6 months after cessation of transfusion. We expect that this result will improve his QOL impaired by long-term transfusion and lessen the risk of morbidity associated with chronic RBC transfusions. Although it is difficult to generalize because this report is on a single case, but this study suggests that TKM treatment can be a meaningful alternative treatment for severe anemia and demonstrates the superiority of Sasang constitutional medicine as a personalized medicine.
Acknowledgment
This study was supported by Ministry of Health & Welfare, Republic of Korea (Grant Number : HI9C1046) and National Research Foundation of Korea (Grant number : NRF-2018R1C1B6007898).