References
1. Korean stroke society. Textbook of stroke 2nd edth ed. Seoul: PanMun education; 2015. 3p. 57–63.
p. 389. p. 527. p. 550.
2. Mercier L, Audet T, Hebert R, Rochette A, Dubois M.-F. Impact of motor, cognitive, and perceptual disorders on ability to perform activities of daily living after stroke. Stroke 2001;32(11):2602–8.
http://doi.org/10.1161/hs1101.098154.
3. Hong KS, Bang OY, Kang DW, Yu KH, Bae HJ, Lee JS, et al. Stroke statistics in Korea: part I. Epidemiology and risk factors: a report from the korean stroke society and clinical research center for stroke. J Stroke 2013;15(1):2–20.
http://doi.org/10.5853/jos.2013.15.1.2.
7. Tuner J, Hode L. Laser Therapy Seoul: JeongDam; 2011. p. 8–9.
p. 104–7.
10. Moskvin SV, Khadartsev AA. Methods of effective low-level laser therapy in the treatment of patients with bronchial asthma (literature review). Biomedicine(Taipei) 2020;10(1):1–20.
http://doi.org/10.37796/2211-8039.1000.
11. Gottschling S, Meyer S, Gribova I, Distler L, Berrang J, Gortner L, et al. Laser acupuncture in children with headache : A double-blind, randomized, bicenter, placebo controlled trial. Pain 2008;137:405–12.
http://doi.org/10.1016/j.pain.2007.10.004.
12. Yi WJ, Zhang L, Wang ZZ, Chu XH, Chen J. Research progress of laser therapy in rehabilitation of stroke patients. LASER JOURNAL 2021;(9)42(9):198–201.
13. Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions Ver 5.1.0 [updated Mar 2011] The Cochrane Collaboration; 2011. Available from
http://handbook.cochrane.org.
14. Higgins JPT, Green S. Analyzing and presenting results. Cochrane handbook for systematic reviews of interventions 4.2.6 Chichester, UK: John Wiley&Sons Inc; 2008. p. 79–165.
15. Kim SY, Park JE, Seo HJ, Lee YJ, Jang BH, Son HJ, et al. NECA’s guidance for undertaking systematic reviews and meta-analyses for intervention National Evidence-based Healthcare Collaborating Agency; 2011. [in Korean].
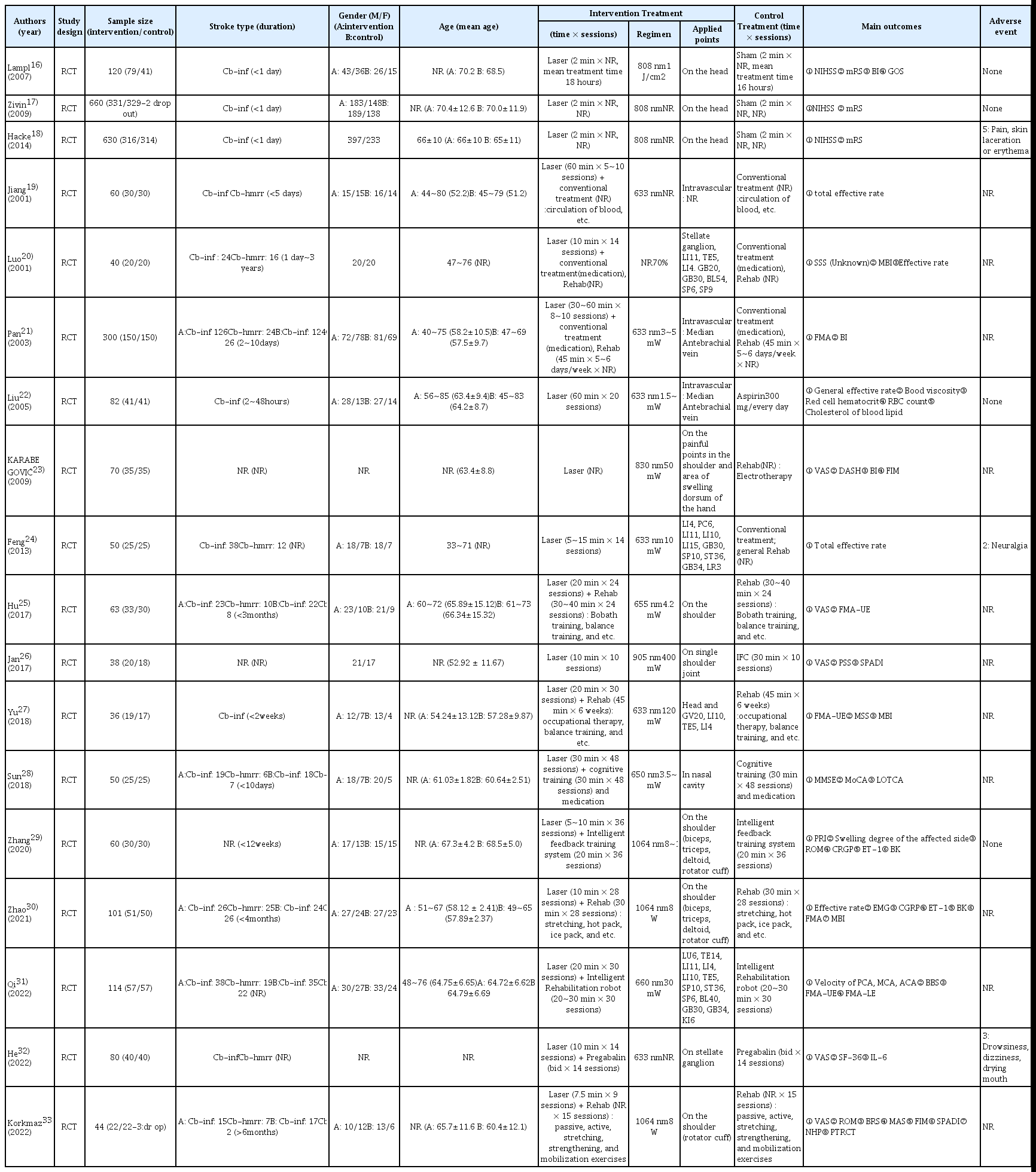
16. Lampl Y, Zivin J, Fisher M, Lew R, Welin L, Dahlof B, et al. Infrared laser therapy for ischemic stroke: a new treatment strategy. Results of the NeuroThera effectiveness and safety trial-1(NEST-1). Stroke 2007;38:1843–9.
http://doi.org/10.1161/STROKEAHA.106.478230.
17. Zivin J, Albers G, Bornstein N, Chippendale T, Dahlof B, Devlin T, et al. Effectiveness and safety of transcranial laser therapy for acute ischemic stroke. Stroke 2009;40(4):1359–64.
http://doi.org/10.1161/STROKEAHA.109.547547.
18. Hacke W, Schellinger PD, Albers GW, Bornstein NM, Dahlof BL, Fulton R, et al. Transcranial Laser Therapy in Acute Stroke Treatment results of Neurothera Effectiveness and Safety Trial 3, a Phase III Clinical End Point Device Trial. Stroke 2014;45(11):3187–93.
http://doi.org/10.1161/STROKEAHA.114.005795.
19. Jiang GF, Zong LQ, Yin YJ, Xuan ZW. Effects of Laser therapy on Dysphagia after Acute Stroke(激光血疗对急性脑卒中后吞咽功能 障碍的疗效评价). Modern Rehabilitation 2001;5(9):62.
21. Pan CH, Pu SX. Effects of Early Intravascular Laser Blood Irradiation and Rehabilitation on Motor Function of Upper and Lower Extremities and Activities of Daily Living in the Patients with Acute Stroke. Chinese Journal of Rehabilitation 2003;18(6):363–4.
22. Liu QS, Wu JX, Liu HL, Hong Li. Effects of He-Ne laser intravascular irradiation on hemorheology and blood lipid of acute cerebral infarction patients. Chinese Journal of Clinical Rehabilitation 2005;9(1):66–9.
23. Azra K, Suada KD, Farid L. Laser therapy of painful shoulder and shoulder-hand syndrome in treatment of patients after the stroke. Bosn J Basic Med Sci 2009;9(1):59–65.
http://doi.org/10.17305/bjbms.2009.2858.
24. Feng YM, Cheng ZP, Sun H, Shi D. Laser acupuncture treatment in stroke patients with hemiplegia Applications. LASER JOURNAL 2013;34(6):70–1.
25. Hu YL, Xiao YH, Liu AM, Hua YP, Huang Y. Effectiveness of Low Level Laser Combined with Shoulder Control Training in the Treatment of Shoulder Pain in Elderly Hemiplegic Patients with Cerebral Hemiplegia (低强度激光结合肩部控制训练治疗老年脑卒中偏 瘫病人肩痛的疗效观察). Practical Geriatrics 2017;31(2):175–7.
26. Jan F, Naeem A, Malik AN, Amjad I, Malik T. Comparison of low level laser therapy and interferential current on post stroke shoulder pain. J Pak Med Assoc 2017;67(5):788–9.
27. Yu HX, Yang CS, Jia J, He L, Wu GY, Zhang R, et al. Effects of laser radiation at acupoint and hand projection areas of brain on hand and upper extremity function of early stroke patients. Chinese Journal of Reha-bilitation Medicine 2018;33(3):315–8.
http://doi.org/10.3969/j.issn.1001-1242.2018.03.012.
28. Sun L, Shen XY, Ye W, Yan S. Curative effectiveness of laser irradiation in nasal cavity for patients with cognitive impairment after stroke. Chinese Journal of Rehabilitation 2018;33(4):272–4.
http://doi.org/10.3870/zgkf.2018.04.002.
29. Zhang NJ, Jin XS, Ji PP. Curative Effect of High Intensity Laser Therapy Combined with Upper Limb Intelligent Feedback Training System on Patients with Complex Regional Pain Syndrome Type I in after Ischemic Stroke. Journal of practical cardiocerebral pulmonary vasculopathy 2020;28(7):120–4.
http://doi.org/10.3969/j.issn.1008-5971.2020.07.022.
31. Qi L, Zhen QX, Liu C, Yan HJ, Liu AX. Effect of semiconductor laser acupoint irradiation combined with intelligent rehabilitation robot on stroke hemiplegia and BBS and FMA scores. Journal of Clinical and Experimental Medicine 2022;21(5):539–42.
http://doi.org/10.3969/j.issn.1671-4695.2022.05.025.
32. He BJ, Xia HT, Liang JQ, Zeng DY, Liang YC, Wang ZQ. Evaluation of the effect of super laser irradiation on stellate ganglion combined with pregabalin in the treatment of central neuralgia after stroke. Journal of China Prescription Drug 2022;20(3):110–2.
http://doi.org/10.3969/j.issn.1671-945X.2022.03.044.
33. Korkmaz N, Gurcay E, Demir Y, Tezen O, Korkmaz İ, Atar MO, et al. The effectiveness of high-intensity laser therapy in the treatment of post-stroke patients with hemiplegic shoulder pain: a prospective randomized controlled study. Lasers Med Sci 2022;37(1):645–53.
http://doi.org/10.1007/s10103-021-03316-y.
34. Park SU, Cho SY, Park JM, Ko CN, Park HJ, Walls B, et al. Integrative treatment modalities for stroke victims in Korea. Complementary Therapies in Clinical Practice 2014;20(1):37–41.
http://doi.org/10.1016/j.ctcp.2013.10.007.
35. Yamashita H, Tsukayama H, Tanno Y, Nishijo K. Adverse events in acupuncture and moxibustion treatment: a six-year survey at a national clinic in Japan. J Altern Complement Med 1999;Jun. 5(3):229–36.
http://doi.org/10.1089/acm.1999.5.229.
36. Siedentopf CM, Koppelstaetter F, Haala IA, Haid V, Rhomberg P, Ischebeck A, et al. Laser acupuncture induced specific cerebral cortical and subcortical activations in humans. Lasers Med Sci 2005;20(2):68–73.
http://doi.org/10.1007/s10103-005-0340-3.
37. Lv J, Shi CH, Deng YJ, Lou WT, Hu j, Shi L, et al. The brain effects of laser acupuncture at thirteen ghost acupoints in healthy individuals: A resting-state functional MRI investigation. Computerized Medical Imaging and Graphics 2016;(12)54:48–54.
http://doi.org/10.1016/j.compmedimag.2016.08.003.