References
1. Central Disease Control Headquarters, Central Disaster Management Headquarters. 2022. The COVID-19 At-Home Treatment Guideline (Ver.7) Korea: Korea Disease Control and Prevention Agency.
2. Kim Y, Kim SE, Kim T, Yun KW, Lee SH, Lee E, et al. 2022;Preliminary Guidelines for the Clinical Evaluation and Management of Long COVID. Infect Chemother 54(3):566–597.
10.3947/IC.2022.0141.
3. Groff D, Sun A, Ssentongo AE, Ba DM, Parsons N, Poudel GR, et al. 2021;Short-term and Long-term Rates of Postacute Sequelae of SARS-CoV-2 Infection: A Systematic Review. JAMA Netw Open 4(10):e2128568. 10.1001/JAMANETWORKOPEN.2021.28568.
4. Kim Y, Bitna-Ha , Kim SW, Chang HH, Kwon KT, Bae S, et al. 2022;Post-acute COVID-19 syndrome in patients after 12 months from COVID-19 infection in Korea. BMC Infect Dis 22(1):93. 10.1186/S12879-022-07062-6.
5. Kim D, Jerng UM, Lee JY. 2022;An Overview of Clinical Features, and Medical Access Among Patients with Post-Acute COVID-19 Syndromes: Analysis of a Nationwide Survey in Korea. Perspect Integr Med 1(1):21–33.
10.56986/PIM.2022.09.005.
6. Kim Y, Kim SW, Chang HH, Kwon KT, Bae S, Hwang S. 2021;Significance and Associated Factors of Long-Term Sequelae in Patients after Acute COVID-19 Infection in Korea. Infect Chemother 53(3):463–476.
10.3947/IC.2021.0022.
7. Hale N, Meit M, Pettyjohn S, Wahlquist A, Loos M. 2022;The implications of long COVID for rural communities. J Rural Health 38(4):945–947.
10.1111/JRH.12655.
8. Lee JH. 2016;The Regional Health Inequity, and Individual and Neighborhood Level Health Determinants. Heal Soc Welf Rev 36(2):345–384.
10.15709/HSWR.2016.36.2.345.
9. An S, Kim N, Kim Y. 2019. Comparison of Health Status and the Effectiveness of Health Cost between Rural and Urban Residents Korea Rural Economic Institute.
10. Pang W, Yang F, Zhao Y, Dai E, Feng J, Huang Y, et al. 2022;Qingjin Yiqi granules for post-COVID-19 condition: A randomized clinical trial. J Evid Based Med 15(1):30–38.
10.1111/JEBM.12465.
11. An X, Peng B, Huang X, Jiang H, Xiong Z, Zhang H, et al. 2022;Ludangshen oral liquid for treatment of convalescent COVID-19 patients: a randomized, double-blind, placebo-controlled multicenter trial. Chin Med 17(1):1–8.
10.1186/S13020-022-00602-X.
12. Jang S, Kim D, Yi E, Choi G, Song M, Lee EK. 2021;Telemedicine and the Use of Korean Medicine for Patients With COVID-19 in South Korea: Observational Study. JMIR Public Heal Surveill 7(1):e20236. 10.2196/20236.
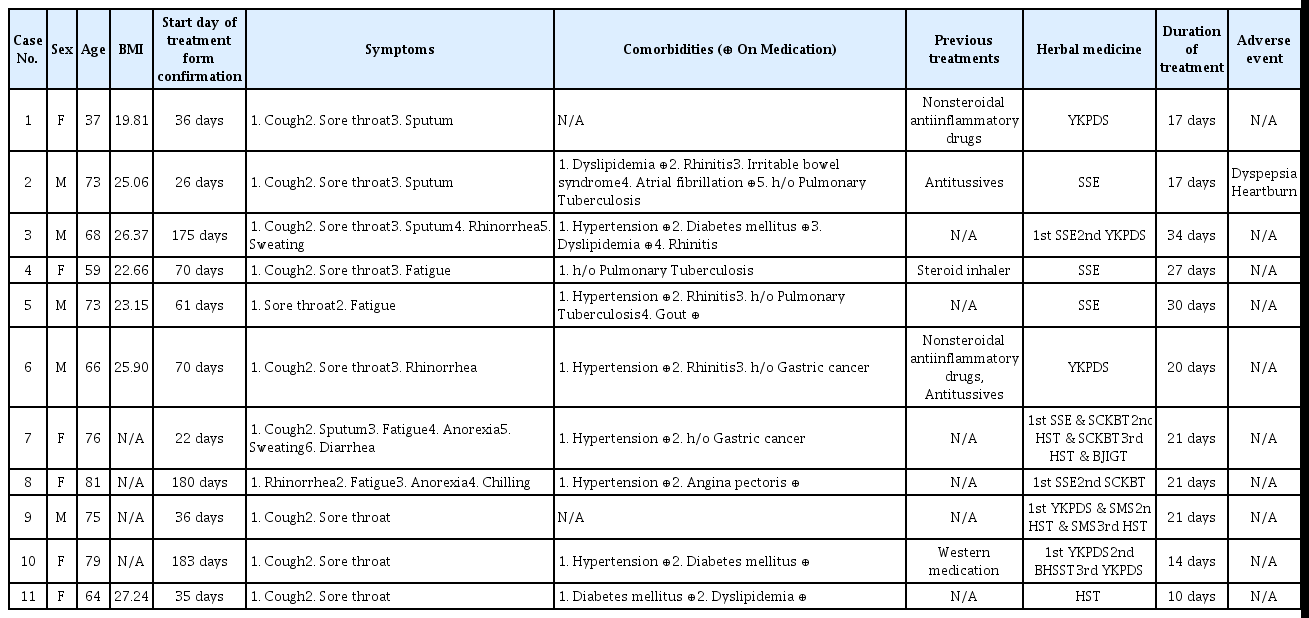
13. Park J, Hong S, Shin JW, Kim KI, Lee BJ, Jung HJ, et al. 2022;Effects of Korean Medicine Treatment in Post-acute COVID-19 Syndrome: A Retrospective Case Series of 15 Patients. J Intern Korean Med 43(3):396–412.
10.22246/JIKM.2022.43.3.396.
14. Jeon C, Choi D, Kim G, Kim H, Leem J, Chi GY, et al. 2022;Effect of Non-contact Korean Medical Treatment for Patients Recovering at Home with Positive Coronavirus Disease 2019 Diagnostic Test Results at a Local Public Health Center: A Retrospective Chart Review. J Physiol Pathol Korean Med 36(4):130–137.
10.15188/KJOPP.2022.08.36.4.130.
15. Yu CH. 2022;A Case Report of a Patient with Long COVID Complaining of Cough and Sore throat Treated with Hyunggaeyungyo-tang and Saengmaek-san. J Korean Med 43(3):204–210.
10.13048/JKM.22041.
18. Su Y, Yuan D, Chen DG, Ng RH, Wang K, Choi J, et al. 2022;Multiple early factors anticipate post-acute COVID-19 sequelae. Cell 185(5):881–895.e20.
10.1016/J.CELL.2022.01.014.
19. Merzon E, Weiss M, Krone B, Cohen S, Ilani G, Vinker S, et al. 2022;Clinical and Socio-Demographic Variables Associated with the Diagnosis of Long COVID Syndrome in Youth: A Population-Based Study. Int J Environ Res Public Health 19(10)10.3390/IJERPH19105993.
20. Tenforde MW, Kim SS, Lindsell CJ, Billig Rose E, Shapiro NI, Files DC, et al. 2020;Symptom Duration and Risk Factors for Delayed Return to Usual Health Among Outpatients with COVID-19 in a Multistate Health Care Systems Network - United States, March–June 2020. MMWR Morb Mortal Wkly Rep 69(30):993–998.
10.15585/MMWR.MM6930E1.
21. Jung YH, Ha EH, Choe KW, Lee S, Jo DH, Lee WJ. 2022;Persistent Symptoms After Acute COVID-19 Infection in Omicron Era. J Korean Med Sci 37(27):e213. 10.3346/JKMS.2022.37.E213.
22. Saunders C, Sperling S, Bendstrup E. 2023;A new paradigm is needed to explain long COVID. Lancet Respir Med 11(2):e12–e13.
10.1016/S2213-2600(22)00501-X.
23. Jiang W, Qi J, Li X, Chen G, Zhou D, Xiao W, et al. 2022;Post-infectious cough of different syndromes treated by traditional Chinese medicines: A review. Chinese Herb Med 14(4):494–510.
10.1016/J.CHMED.2022.09.002.
24. Song WJ, Kim SH. 2019;New Approach to Chronic Cough: An Introductory Guide Based on Recent Clinical Practice Guidelines. Korean J Med 94(6):471–484.
10.3904/KJM.2019.94.6.471.
25. Vijayakumar B, Boustani K, Ogger PP, Papadaki A, Tonkin J, Orton CM, et al. 2022;Immuno-proteomic profiling reveals aberrant immune cell regulation in the airways of individuals with ongoing post-COVID-19 respiratory disease. Immunity 55(3):542–556.e5.
10.1016/J.IMMUNI.2022.01.017.
26. McMaster SR, Wilson JJ, Wang H, Kohlmeier JE. 2015;Airway-Resident Memory CD8 T Cells Provide Antigen-Specific Protection against Respiratory Virus Challenge through Rapid IFN-γ Production. J Immunol 195(1):203–209.
10.4049/JIMMUNOL.1402975.
27. Deng Z, Zhou W, Sun J, Li C, Zhong B, Lai K. 2018;IFN-γ Enhances the Cough Reflex Sensitivity via Calcium Influx in Vagal Sensory Neurons. Am J Respir Crit Care Med 198(7):868–879.
10.1164/RCCM.201709-1813OC.
28. Sun J, Zhan C, Deng Z, Luo W, Chen Q, Jiang M, et al. 2022;Expression of interferon-γ and its effect on cough hypersensitivity in chronic refractory cough patients. Thorax 77(6):621–624.
10.1136/THORAXJNL-2021-218403.
29. Phetsouphanh C, Darley DR, Wilson DB, Howe A, Munier CML, Patel SK, et al. 2022;Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection. Nat Immunol 23(2):210–216.
10.1038/S41590-021-01113-X.
30. Krishna B, Lim E, Mactavous L, Jackson S, Lyons P, Bradley J, et al. 2022;Spontaneous, persistent T-cell dependent IFN-γ release in patients who progress to Long COVID. Prepr (Version 2) available Res Sq Published online November 21, 2022. 10.21203/RS.3.RS-2034285/V2.
31. Kim YC, Song WJ. 2022;Neuro-Immune Interactions and IFN-γ in Post-Infectious Cough. Allergy Asthma Immunol Res 14(6):581–584.
10.4168/AAIR.2022.14.6.581.
32. De Araujo-Souza PS, Hanschke SCH, Viola JPB. 2015;Epigenetic control of interferon-gamma expression in CD8 T cells. J Immunol Res 2015;:849573. 10.1155/2015/849573.
33. Kaech SM, Cui W. 2012;Transcriptional control of effector and memory CD8+ T cell differentiation. Nat Rev Immunol 12(11):749–761.
10.1038/NRI3307.
34. Szabo SJ, Kim ST, Costa GL, Zhang X, Fathman CG, Glimcher LH. 2000;A novel transcription factor, T-bet, directs Th1 lineage commitment. Cell 100(6):655–669.
10.1016/S0092-8674(00)80702-3.
35. Drae Yoon, Sin Hong, Hin Noh, Sra Yi, Ihee Lee, Jhwan Lew, et al. 2013;Observation of Inflammatory Marker Levels in Sprague-Dawley Rats with Youngyopaedoc-san-related Anti-atherogenic Effect. J Korean Med 34(3):86–95.
10.13048/jkm.13014.
36. KIM JB, Kang H, Ahn KS, Sang SB, Sung-Hoon K, Seung-hoon C, et al. 2009;Effect of Soyangin-Hyeongbangpaedok-san on Anti-CD3 Stimulated Mouse T Cells In Vivo and In Vitro. J Physiol Pathol Korean Med 23(3):554–561.
37. Kim HJ, Han HJ, Jang JA, Park EY, An TH, Seo HS, et al. 2010;Clinic Study on Herb Medication for Patients Who have a Chronic Respiratory Disease from the Cold Sequelae. J Herb Formula Sci 18(1):181–189.
38. Ryu NH, Park S, Kang H, Sang SB, Sung-Hoon K, Seung-hoon C, et al. 2008;Effect of Samsoeum on Cytokine Regulation of Mouse T cell. J Physiol Pathol Korean Med 22(4):856–862.
39. Tang WF, Tsai HP, Chang YH, Chang TY, Hsieh CF, Lin CY, et al. 2021;Perilla (Perilla frutescens) leaf extract inhibits SARS-CoV-2 via direct virus inactivation. Biomed J 44(3):293–303.
10.1016/J.BJ.2021.01.005.
40. Rhee SH, Kang MS, Choi YK, Jun CY, Park CH, Kim DW. 2006;Comparative study of 202 herbs on interferon-gamma secretion. J Intern Korean Med 27(2):336–344.
41. Shin YS, Liu JN, Kim JH, Nam YH, Choi GS, Park HS. 2014;The Impact of Asthma Control on Salivary Cortisol Level in Adult Asthmatics. Allergy Asthma Immunol Res 6(5):463–466.
10.4168/AAIR.2014.6.5.463.
42. Wei P, Li Y, Wu L, Wu J, Wu W, Chen S, et al. 2021;Serum cortisol levels and adrenal gland size in patients with chronic obstructive pulmonary disease. Am J Transl Res 13(7):8150–8157.
43. Landstra AM, Postma DS, Marike Boezen H, Van Aalderen WMC. 2002;Role of serum cortisol levels in children with asthma. Am J Respir Crit Care Med 165(5):708–712.
10.1164/AJRCCM.165.5.2102115.
44. Choi SY, Han SW. 1990;Effects of PaiMo-San water extract on the plasma cortisol concentraction and arterial blood PCO2, PO2 in the rabbit. J Intern Korean Med 11(1):127–140.
45. Vink NM, Boezen HM, Postma DS, Rosmalen JGM. 2013;Basal or stress-induced cortisol and asthma development: the TRAILS study. Eur Respir J 41(4):846–852.
10.1183/09031936.00021212.
46. The whole country a college of Orental medicine. The joint textbook publish commission compilatioin. 2011. Herbology 2nd edth ed. Yonglimsa.
47. Kang WJ, Seo UK. 2008;Effects of Haengso-tang and Chwiyeon-tang on Expression of Respiratory Mucin Gene and Secretion of Airway Mucus. J Korean Med 29(3):76–87.
49. Lee K, Jeong S, Jeong M, Choi Y, Song M, Jang I. 2021;Review on Herbal Medicine Treatment for Late Complications of COVID-19 Patients. J Intern Korean Med 42(1):53–66.
10.22246/JIKM.2021.42.1.53.
50. Kim D, Park SH, Sung WS, Kim EJ. 2022;Current Status of Korean Medicine Treatment for Post-acute COVID-19 Syndrome: A Survey of Korean Medicine Doctors. Perspect Integr Med 1(1):34–44.
10.56986/PIM.2022.09.006.